Abstract
Introduction: To compare the effects of oral clonidine and tramadol on shivering caused by spinal anesthesia in patients undergoing transurethral lithotripsy (TUL).
Methods: The present study is a triple-blind clinical trial conducted on 80 elective urologic surgical candidates during 2016-2017 at Tehran Hasheminejad Hospital in Iran. Using the Balanced Block Randomization method, the patients were randomly assigned into two groups (40 patients per group) 90 minutes before performing spinal anesthesia. The first group (group C) received 150 µg of oral clonidine and the second group (group T) received 50 mg of oral tramadol. Body temperature, core body temperature, heart rate, diastolic blood pressure and shivering were recorded for the patients at different time periods, and entered in the SPSS22 software program. The above variables were then statistically analyzed using independent sample T-tests chi-squared tests and Repeated Measure ANOVA.
Results: The results of this study indicated that there was a significant statistical difference (P<0.05) between the clonidine and tramadol treatment groups with regards to some variables, such as average body temperature and average core temperature, at different time periods. However, for other variables, such as heart rate, systolic blood pressure, diastolic blood pressure and shivering, there were no significant statistical differences between the two treatment groups (P>0.05).
Conclusion: Clonidine and tramadol treatment groups were only significantly different in terms of body temperature and core temperature. Therefore, it is recommended that other precise randomized clinical trials be performed to ensure the accuracy of the results of this study.
Introduction
Postanesthetic shivering is one of the most common postoperative complications. It involves involuntary movements of one or more groups of muscles and its prevalence varies from 3.6 to 65% Hemmati et al., 2014. Shivering is defined as detectable fasciculation and tremor in the face, jaw, head, trunk and limbs, lasting more than 15 seconds Panzer et al., 1999. Shivering is an involuntary muscle movement which sharply raises basal metabolism. It is induced when the preoptic area of the hypothalamus senses that the body is too cold. Postanesthetic shivering consists of involuntary muscular contractions and movements which the patient has no control over; it is easily identifiable but if left untreated, may last many minutes or even hours after the operation is performed Buggy and Crossley, 2000De Witte and Sessler, 2002.
Just like nausea and vomiting, postanesthetic shivering is an unpleasant complication of anesthesia. Although the cause of this complication still remains unknown, most of its adverse effects are well understood Alfonsi, 2003Macario et al., 1999. It may result from intraoperative hypothermia (due to regulation of core body temperature) or secondary chills (due to activation of inflammatory response and cytokine release) Yared et al., 1998. In terms of its adverse effects, postoperative shivering may lead to increased oxygen consumption, increased production of carbon dioxide, exacerbation of ischemic heart disease (due to increased heart rate and blood pressure), increased intracranial pressure, increased intraocular pressure, and increased pain in the surgical site (due to stretching of the incision). Furthermore, shivering may interfere with the patient monitoring process.
Since shivering, like other complications of anesthesia, can lead to patient dissatisfaction, increased morbidity during and after surgery, and increased oxygen consumption (up to 600%), appropriate measures should be implemented both before and during surgery to reduce its prevalence. Nowadays, many different pharmacological and non-pharmacological measures are taken to prevent hypothermia and shivering. Keeping the patient warm before and during surgery as well as preventing the operating room from getting cold are some important non-pharmacological methods. Administering oxygen, keeping the patient warm, and controlling spinal reflexes have great impact on controlling shivering Davis and Bissonnette, 1999Kranke et al., 2004.
On the other hand, since the entire skin surface area is involved in controlling the body temperature by 20%, non-pharmacological methods are not adequate to control shivering and, therefore, it is necessary to use pharmacological methods as well. Today, the use of medications is still the best known method for prevention and treatment of postoperative shivering. Given that several mechanisms are involved in preventing shivering, several medications (such as meperidine, tramadol, hydrocortisone, nefopam, clonidine, ketamine, and magnesium sulfate) have been used to treat shivering. The mechanism of action of each of these medications is different. For instance, pethidine controls shivering through affecting the kappa receptor or having a direct impact on the heat-regulating center. Tramadol acts through the inhibiting the re-uptake of 5-hydroxytryptamine (5-HT, serotonin), norepinephrine and dopamine; as well, easing the release of tramadol inhibits shivering Davoudi et al., 2009Honarmand and Safavi, 2008Pawar et al., 2011Vanderstappen et al., 1996Wang et al., 1999.
Use of these medications may lead to some unwanted complications. As an example, meperidine (pethidine) which is one of the most common medications used to treat postanesthetic shivering, has been reported to induce such complications as tachycardia, agitation, dizziness, chemical dependency, delirium, hallucinations, seizure and Parkinson's disease. These complications have led researchers to conduct studies in this field to attempt to find alternative medications Hoseinkhan and Behzadi, 2006. Therefore, it is important to consider the importance of controlling postanesthetic shivering while also considering the selection and prescription of the most suitable pharmacological treatment. The goal of this study was to compare the oral effects of clonidine and tramadol on prevention of shivering resulting from spinal anesthesia.
Materials-Methods
This study has been approved by the Ethics Committee of Iran University of Medical Sciences. The present study is a triple-blind randomized clinical trial conducted on 80 elective urologic surgical candidates, of ages ranging from 18-70 years, in Hasheminejad Hospital during 2016-2017. The patients were included in the first or second classification of the American Society of Anesthesiologists (ASA). Using Balanced Block Randomization method, these patients were assigned into two groups: Tramadol (T) and Clonidine (C) treatment groups. Ninety minutes before spinal anesthesia, group C received 150 µg of oral clonidine while group T received 50 mg of oral tramadol.
The exclusion criteria were history of seizure, hypo- or hyper-thyroidism, cardiopulmonary diseases, psychiatric disorders, musculoskeletal disorders, allergies to the study medications, primary heart rate of <50 beats per minute, systolic blood pressure of <100 mm Hg, and body temperature of >38 or <36°C before conducting spinal anesthesia.
In this study, shivering was evaluated with the use of the Crossley and Mahajan scale. The evaluations were recorded within 10 minutes after conducting spinal anesthesia. Body and tympanic membrane temperatures were recorded with a mercury thermometer and Microlife ear digital thermometer, respectively, at the beginning of shivering and within 5, 10 and 20 minutes after shivering. All of the surgeries were conducted in the operating room of temperature between 19-21°C, while humidity was maintained at approximately 60%.
None of the patients received medications other than the study medications (which were received as prodrugs). Standard monitoring, including ECG, pulse oximeter and blood pressure, were performed for all patients. Subarachnoid anesthesia was carried out in lumber spine L3-L4 or L4-L5 disc with 15 mg of hyperbaric bupivacaine. Intravenous fluids and ephedrine for hypotension cases, atropine for bradycardia cases, and metoclopramide for nausea and vomiting cases, were prescribed and administered by an anesthesiologist, in the form of 10 mg injected slowly i.v. Administration of opioid was avoided both before anesthesia and during the procedure. Before undergoing spinal anesthesia, the patients received 10 mg/kg of crystalloid. Also, during the procedure 6 mg/kg of crystalloid, as maintenance fluid, was administered to the patients. The patients were also backed with 5 liters of oxygen per minute. A layer of surgical drapes was used in the surgical area and a layer of linen fabrics was used for covering non-surgical areas. All fluids administered to the patients were at the temperature of 37oC. Written informed consent from the patients was obtained before conducting the study, which incidentally was registered in the Iranian Clinical Trials Center (IRCT201410275168N9code).
The data gathering tool, in the present study, was a checklist for variables-including age, sex, body temperature, core body temperature, heart rate, systolic blood pressure, diastolic blood pressure, and shivering- at different time points. The collected data were then entered into the SPSS Statistics V22.0 software program, and analyzed via chi-squared tests, independent sample t-tests, and Repeated Measure ANOVA tests.
Results
The mean age of patients in the tramadol and clonidine treatment groups were 43.55±11.91 and 41.83±13.31, respectively; this difference was not statistically significant (P=543.0; t-test). In the present study, 72.5% and 80% of the patients in the Tramadol and Clonidine groups, respectively, were men. The gender difference between the two groups was not statistically significant (P= 0.431; chi-square). Moreover, the results of this study showed no significant statistical difference between the two groups (Tramadol and Clonidine) in terms of the variables of atropine, ephedrine, and pethidine (P>0.05). The lack of significant differences in age and sex between the two groups suggests the evidence of a true randomization process.
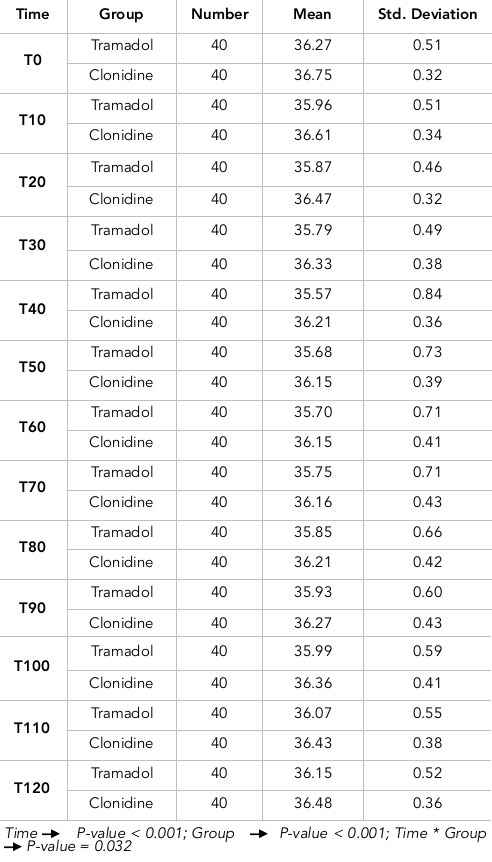
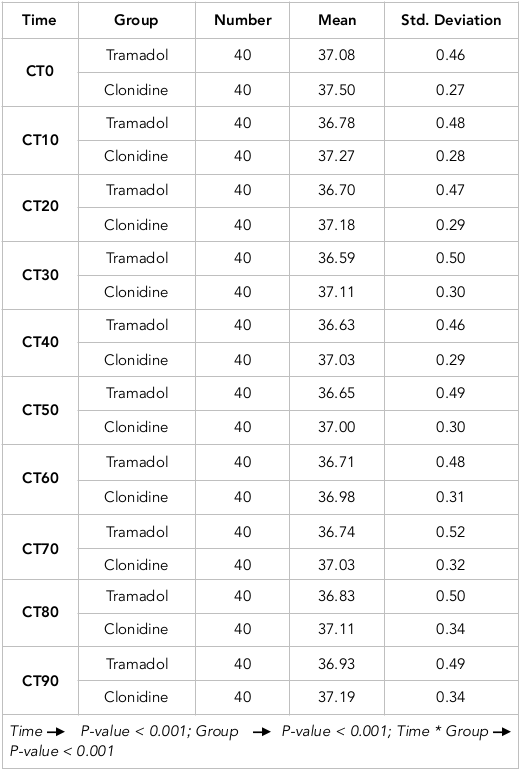
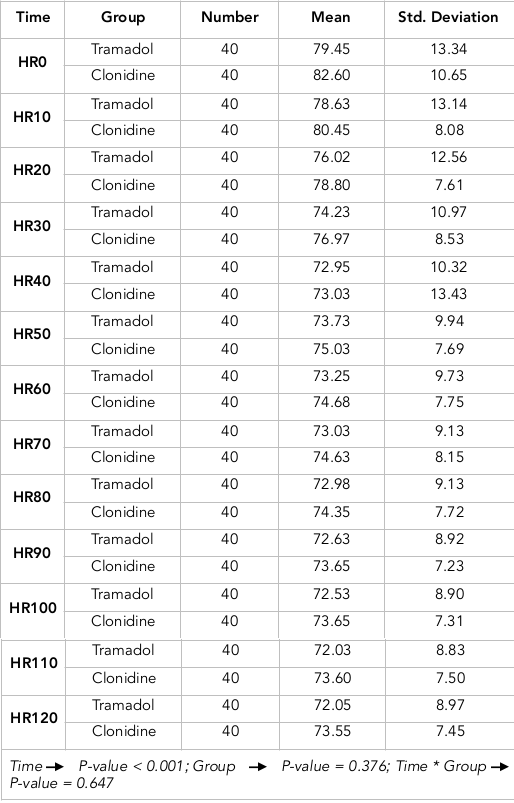
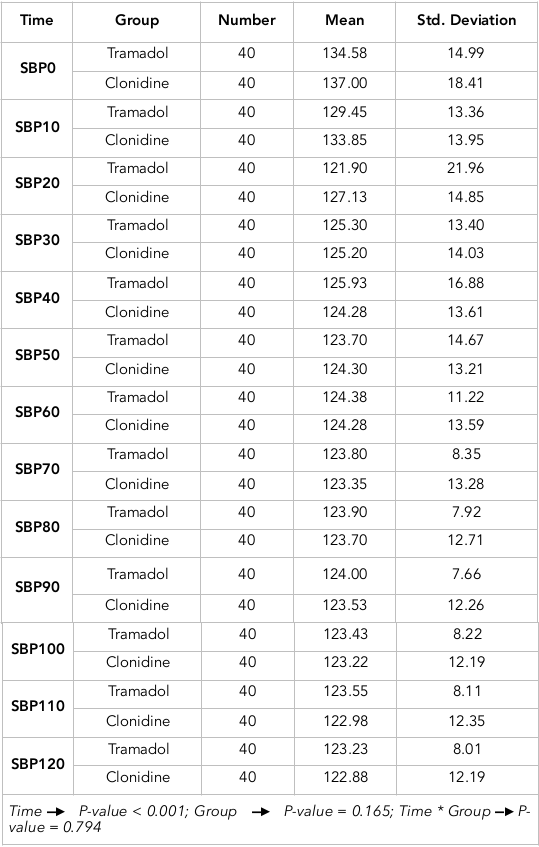
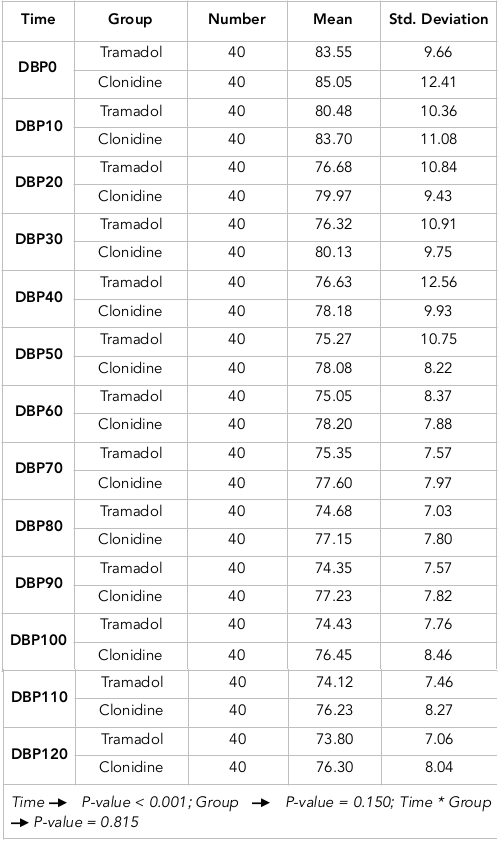
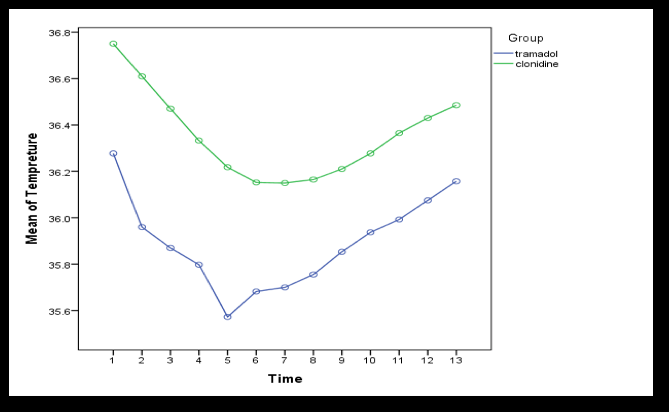
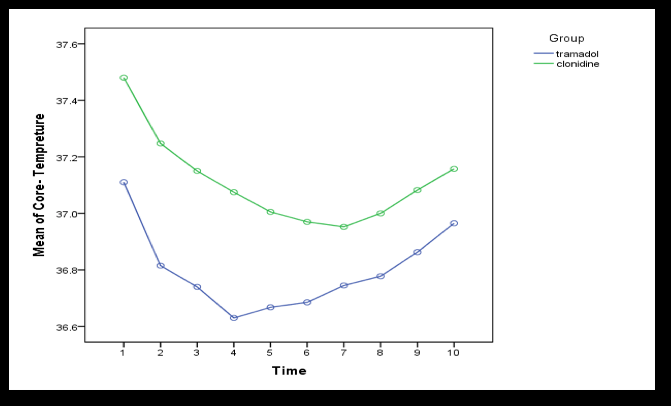
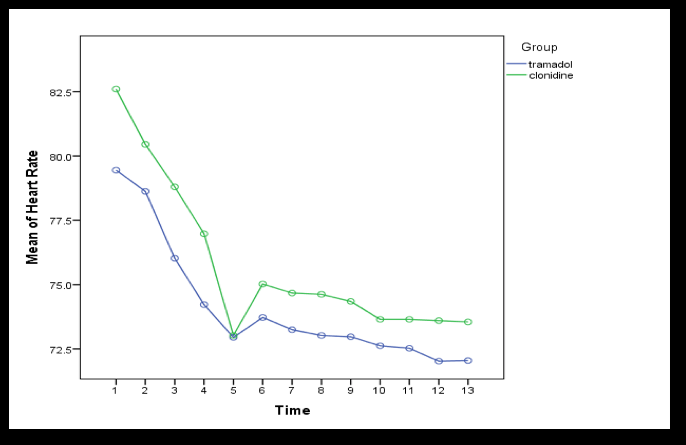
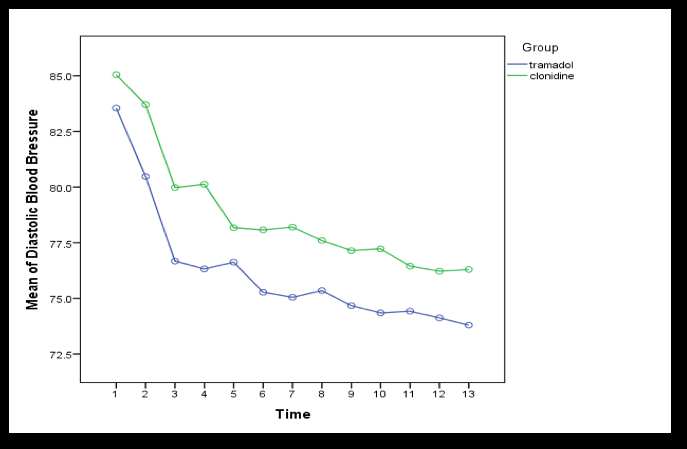
Considering the quantitative nature of the data and their normal distribution, a Repeated Measure ANOVA test was used to compare the means of body temperature, core body temperature, heart rate, systolic blood pressure, and diastolic blood pressure between the two groups (Tramadol and Clonidine) at different time periods. Tables 1-5 show the means of body temperature, core body temperature, heart rate, and systolic and diastolic blood pressure between the two groups (Tramadol and Clonidine) at different time points. Analysis of the results for each variable indicate that only the mean body temperature and mean core body temperature of the treatment groups were significantly different (P=0.032 and P=0.001, respectively). Moreover, for all the time points analyzed, the mean body temperature and mean core body temperature in the Clonidine group were higher than in the Tramadol group. However, there was not any observed statistical difference in the treatment groups for the other variables, such as heart rate, systolic blood pressure, and diastolic blood pressure (P>0.05); Figures 1-5 demonstrate these results.
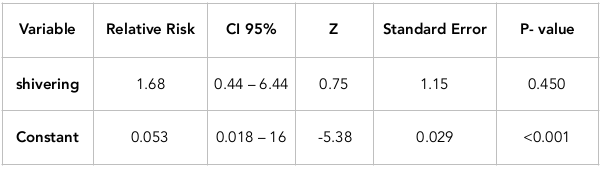
Due to the fact that shivering is a qualitative variable, a Generalized Estimating Equation was used to compare shivering between the two groups (Tramadol and Clonidine) at different time points. The results of this comparison are shown in Table 6 ; as seen, there is no significant statistical difference between the two groups in terms of Relative Risk (RR). In the other words, incidences or risks of shivering in the Tramadol and Clonidine groups are similar at the different time periods (P=0.450).
Discussion
The present study is a randomized clinical trial designed and carried out with the aim of comparing the effects of oral clonidine and tramadol on shivering caused by spinal anesthesia in patients undergoing transurethral lithotripsy (TUL) surgery at the Shahid Hasheminejad Hospital (Iran) from 2016 to 2017. The results of our study indicate that there was no significant statistical difference between the Tramadol and Clonidine treatment groups in terms of the variables of atropine, ephedrine, and pethidine (P>0.05). Also, the only significant statistical difference between the two groups was related to the variables of mean body temperature and mean core body temperature at different time periods (P<0.05). However, there was no significant statistical difference between the two groups in terms of the other variables such as heart rate, systolic blood pressure, diastolic blood pressure and shivering (P>0.05).
In the present study, there was a significant statistical difference between the two groups (Tramadol and Clonidine) with respect to mean body temperature and mean core body temperature (P<0.05); in fact, the overall mean body temperature and mean core body temperature in the Clonidine group were higher than in the Tramadol group. These findings are not consistent with the randomized clinical trial carried out by Emadi et al. who compared the effects of tramadol and pethidine for controlling shivering after surgery and general anesthesia; in their study, there was no observed significant statistical differences between the two groups in terms of the patients' temperature in preanesthetic stage, during surgery, or after shivering incidence Rafeie et al., 2006. In a double-blinded clinical trial conducted by Rama Wilson et al. to compare the effects of Tramadol, Ketamine, and Clonidine on preventing postanesthetic shivering in patients undergoing abdominal and lower extremities surgery, a significant statistical difference was observed only between the three groups and the forth group (control group) in terms of core body temperature. However, there was no significant statistical difference between the three groups in terms of mean core body temperature Wason et al., 2012.
Moreover, in a study by Velayudha S. Reddy et al. to compare the effect of Clonidine and Tramadol on spinal anesthesia-related shivering in cesarean section, the findings indicated that there was no significant statistical difference between the groups in terms of body temperature; the mean body temperature in the Tramadol and Clonidine groups were 37.05±0.2 and 37.04±0.21, respectively Reddy and Chiruvella, 2011. Our findings may be different from these above studies due to differences in dosage of the prescribed drugs, in the characteristics of the study subjects, and in study sample size. Thus, conducting studies with larger sample sizes and prescribing different doses of the drugs could help clarify these issues.
Furthermore, in our study there was no significant statistical difference between the Tramadol and Clonidine groups in terms of the other variables (heart rate, systolic blood pressure, diastolic blood pressure, and shivering (P>0.05)). These findings are consistent with some other studies carried out in this field. For instance, a study conducted by Imani et al. on 60 cholecystectomy candidates evaluated the effects of prescribing oral clonidine before anesthesia on postanesthetic shivering. This study found no significant statistical difference between the Oral Clonidine and Placebo groups in terms of oxygen saturation, pulse, pulse rate, average blood pressure, and time of awakening from anesthesia Khajavi et al., 2012. In other words, it can be concluded that oral types of the drugs result in no particular complications. The lack of complications may be due to slow absorption of the medications when administered orally.
Indeed, the results of our study and the observed lack of significant difference between the Clonidine and Tramadol groups with respect to shivering incidence are inconsistent with results of many other studies conducted in this area. For instance, there was a randomized clinical trial conducted by Prerna Attal et al., on patients undergoing abdominal and lower extremities surgery, to compare the effect of Clonidine and Tramadol on spinal anesthesia-related shivering. Their findings indicated that the time required for stopping shivering and improving the patients’ condition was significantly lower in the Tramadol group (3.16±0.84 min) than the Pethidine group (5.76±0.8 min); yet, there was no significant statistical difference between the Tramadol and Clonidine groups in terms of heart rate, systolic blood pressure, and diastolic blood pressure Attal et al., 2015.
Moreover, a study carried out by Billotta et al., conducted on 101 patients undergoing anesthesia, indicated that in comparison to placebo, clonidine significantly reduced the incidence of shivering Bilotta et al., 2005. A systematic and quantitative review study conducted in 27 clinical trials showed that clonidine, in different doses, was effective at reducing placebo-related shivering Kranke et al., 2004. Studies also show that clonidine alpha-2 receptor agonist is located in central and peripheral nervous systems and its most important central effect is its sedative and analgesic impacts.
Clonidine reduces blood pressure and bradycardia through decreasing sympathetic activities and increasing parasympathetic activities. After oral administration, clonidine is completely and quickly absorbed; its maximum plasma level is 60-90 unit. Complications of clonidine consumption are usually mild. Due to their anti-anxiety effects, alpha-2 agonists are good supplements for anesthetics and analgesics Crassous et al., 2007Moodi and Borjian, 2009. Also, other studies have shown that tramadol is a new synthetic opioid with characteristics of a receptor μ antagonist; it can inhibit the uptake of norepinephrine, dopamine and serotonin in the central nervous system. It acts through the mechanisms of regulating temperature and modulating anti-shivering effects.
Although there are different research studies evaluating the role of tramadol in postanesthetic shivering, due to the different characteristics of patients different results have been reported Eberhart et al., 2005Tsai and Chu, 2001. Our study is different from other studies in that we observed that the clonidine and tramadol do not differ in terms of controlling shivering. We must take into consideration the limited studies that have directly compared the effects of tramadol and clonidine in controlling shivering. It is recommended that more detailed studies with larger sample sizes be designed and carried out to compare tramadol and clonidine at different doses to help clarify the issue. Indeed, a limitation of our study was the limited number of ASA I and II patients undergoing TUL at the Shahid Hasheminejad Hospital; most of these patients were suffering from heart and kidney disorders and considered to be ASA III patients. Nonetheless, clonidine and tramadol treatment groups showed significant differences in mean body temperature and mean core body temperature. It is recommended that other precise randomized clinical trials be performed to further explore these findings.
Conclusion
Clonidine and tramadol treatment groups were only significantly different in terms of body temperature and core temperature. Therefore, it is recommended that other precise randomized clinical trials be performed to ensure the accuracy of the results of this study.
Abbreviations
ASA: American Society of Anesthesiologists
GEE : Generlized Estimating Equation
RR : Relative Risk
TUL: Trans Ureteral Lithotripsy
Author Contribution
SFM, MRM and GHM designed the study. MMK, MGH , AM and MM processed the data. SFM, MRM and MMK performed the statistical analysis. AM, MM and GHM interpreted the results. SFM, MRM, GHM and MGH wrote the first draft. SFM, MRM , AM and MM revised the final draft. All authors read and approved the final manuscript.
References
-
P.
Alfonsi.
Postanaesthetic shivering. Epidemiology, pathophysiology and approaches to prevention and management. Minerva Anestesiologica.
2003;
69(5)
:
438-442
.
-
P.
Attal,
A.
Chhaya,
T.
Singh,
R.
Upadhayaya.
Comparison of clonidine and tramadol for the control of shivering under spinal anaesthesia . International Journal of Biomedical and Advance Research.
2015;
6(1)
:
25-31
.
View Article Google Scholar -
F.
Bilotta,
F.
Ferri,
F.
Giovannini,
G.
Pinto,
G.
Rosa.
Nefopam or clonidine in the pharmacologic prevention of shivering in patients undergoing conscious sedation for interventional neuroradiology . Anaesthesia.
2005;
60(2)
:
124-128
.
View Article Google Scholar -
D.
Buggy,
A.
Crossley.
Thermoregulation, mild perioperative hypothermia and post-anaesthetic shivering . British Journal of Anaesthesia.
2000;
84(5)
:
615-628
.
View Article Google Scholar -
P.-A.
Crassous,
C.
Denis,
H.
Paris,
J. M.
Sénard.
Interest of α2-adrenergic agonists and antagonists in clinical practice: Background, facts and perspectives . Current Topics in Medicinal Chemistry.
2007;
7(2)
:
187-194
.
View Article Google Scholar -
A. J.
Davis,
B.
Bissonnette.
Thermal regulation and mild intraoperative hypothermia . Current Opinion in Anaesthesiology.
1999;
12(3)
:
303-309
.
View Article Google Scholar -
M.
Davoudi,
S. H.
Mousavi-Bahar,
A.
Farhanchi.
Intrathecal meperidine for prevention of shivering during transurethral resection of prostate. Urology Journal.
2009;
4(4)
:
212-216
.
-
J.
De Witte,
D. I.
Sessler.
Perioperative ShiveringPhysiology and Pharmacology. The Journal of the American Society of Anesthesiologists.
2002;
96(2)
:
467-484
.
-
L. H.
Eberhart,
F.
Döderlein,
G.
Eisenhardt,
P.
Kranke,
D. I.
Sessler,
A.
Torossian.
Independent risk factors for postoperative shivering . Anesthesia and Analgesia.
2005;
101(6)
:
1849-1857
.
View Article Google Scholar -
K.
Hemmati,
E.
Derikvand,
A.
Delpisheh,
M.
Safari.
Comparison between effects of different doses of pethidine and fentanyl on shivering after spinal anesthesia in orthopedic patients referred to Imam Khomeini Hospital (RH) of Ilam. Anesthesiology and Pain.
2014;
4(4)
:
40-48
.
-
A.
Honarmand,
M.
Safavi.
Comparison of prophylactic use of midazolam, ketamine, and ketamine plus midazolam for prevention of shivering during regional anaesthesia: A randomized double-blind placebo controlled trial . British Journal of Anaesthesia.
2008;
101(4)
:
557-562
.
View Article Google Scholar -
Z.
Hoseinkhan,
M.
Behzadi.
Morphine, Pethidine and Fentanyl in post-operative shivering control: A randomized clinical trial. Tehran University Medical Journal TUMS Publications.
2006;
64(12)
:
57-63
.
-
Mr.
Khajavi,
R.
Shariat‐Moharari,
F.
Imani,
F.
Etezadi.
Evaluation of oral clonidine effects on prevention ofpost-anesthesia shivering. Anesthesiology and Pain.
2012;
2(7)
:
96-0
.
-
P
Kranke,
LH
Eberhart,
N
Roewer,
MR
Tramèr.
Postoperative shivering in children. Pediatric drugs.
;
2003;5(6)
:
373-83
.
-
P.
Kranke,
L. H.
Eberhart,
N.
Roewer,
M. R.
Tramèr.
Single-dose parenteral pharmacological interventions for the prevention of postoperative shivering: A quantitative systematic review of randomized controlled trials . Anesthesia and Analgesia.
2004;
99(3)
:
718-727
.
View Article Google Scholar -
A.
Macario,
M.
Weinger,
S.
Carney,
A.
Kim.
Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesthesia and Analgesia.
1999;
89(3)
:
652
.
-
Z.
Moodi,
S.
Borjian.
A survey on the effect of clonidine in prevention of shivering following general anesthesia. Journal of Birjand University of Medical Sciences.
2009;
16(2)
:
5-9
.
-
O.
Panzer,
N.
Ghazanfari,
D. I.
Sessler,
Y.
Yucel,
M.
Greher,
O.
Akca.
Shivering and shivering-like tremor during labor with and without epidural analgesia. The Journal of the American Society of Anesthesiologists.
1999;
90(6)
:
1609-1616
.
-
MS
Pawar,
N
Suri,
N
Kaul,
S
Lad,
RM
Khan.
Hydrocortisone reduces postoperative shivering following day care knee arthroscopy. Canadian Journal of Anesthesia/Journal canadien d'anesthésie.
;
2011;58(10)
:
924
.
-
M
Rafeie,
S
Hashemi,
A
DAVOUDABADI,
HM
ADIB.
The Study of Effects of Tramadol and Pethidine for Post Operative Shivering after Spinal Anesthesia for Inguinal Hernia Repair in Shahid Beheshti Hospital of Kashan During 18 Months. 2006
.
-
V. S.
Reddy,
S.
Chiruvella.
Clonidine versus tramadol for post spinal shivering during caesarean section: A randomized double blind clinical study. Journal of Obstetric Anaesthesia and Critical Care.
2011;
1(1)
:
26
.
-
Y.-C.
Tsai,
K.-S.
Chu.
A comparison of tramadol, amitriptyline, and meperidine for postepidural anesthetic shivering in parturients . Anesthesia and Analgesia.
2001;
93(5)
:
1288-1292
.
View Article Google Scholar -
I.
Vanderstappen,
E.
Vandermeersch,
B.
Vanacker,
M.
Mattheussen,
P.
Herijgers,
H.
Aken.
The effect of prophylactic clonidine on postoperative shivering . Anaesthesia.
1996;
51(4)
:
351-355
.
View Article Google Scholar -
J.-J.
Wang,
S.-T.
Ho,
S.-C.
Lee,
Y.-C.
Liu.
A comparison among nalbuphine, meperidine, and placebo for treating postanesthetic shivering . Anesthesia and Analgesia.
1999;
88(3)
:
686-689
.
View Article Google Scholar -
R.
Wason,
N.
Jain,
P.
Gupta,
A. R.
Gogia.
Randomized double-blind comparison of prophylactic ketamine, clonidine and tramadol for the control of shivering under neuraxial anaesthesia . Indian Journal of Anaesthesia.
2012;
56(4)
:
370
.
View Article Google Scholar -
J.-P.
Yared,
N. J.
Starr,
L.
Hoffman-Hogg,
C. A.
Bashour,
S. R.
Insler,
M.
O’connor.
Dexamethasone decreases the incidence of shivering after cardiac surgery: A randomized, double-blind, placebo-controlled study. Anesthesia and Analgesia.
1998;
87(4)
:
795-799
.
Comments
Downloads
Article Details
Volume & Issue : Vol 4 No 10 (2017)
Page No.: 1716-1732
Published on: 2017-10-29
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 9888 times
- Download PDF downloaded - 2339 times
- View Article downloaded - 12 times
 Biomedpress
Biomedpress