Significance of p53, pRb and Ki-67 markers in Cervical intraepithelial lesion and Malignancy
Abstract
OBJECTIVE: To study and to derive the significance of expression of p53, pRb and Ki-67 markers in various grades of cervical intraepithelial lesions and malignancy in a tertiary hospital situated in southern part of India which caters the rural and semi-urban population.
METHODS: A total of 120 cervical tissue samples were included. These represented normal, dysplasia and malignancy. Immunohistochemical staining was performed for p53, Ki-67 and pRb in formalin-fixed, paraffin-embedded tissue sections of the uterine cervix using horse-peroxidase method. Descriptive statistical analysis was done; significance was assessed at 5% level of significance. The mean value of the markers was compared between normal and pathological lesions separately using Independent “t” test.
RESULTS: There was significant association of p53 expression between normal cervical epithelium and low grade squamous intraepithelial lesion (LSIL) (p=0.023), squamous cell carcinoma (SCC) (p<0.001) and adenocarcinoma AC (p=0.004), but no significant association with high grade squamous intraepithelial lesion (HSIL) (p=0.09). In case of pRb(n) (n=nuclear) expression significant association was found when normal was compared with LSIL (p<0.001) and HSIL (p=0.001), no association was found with SCC (p=0.207) and AC (p=0.322). pRb(c) (c=cytoplasmic) expression showed significant association when normal was compared with HSIL(p=0.03), SCC (p<0.001) and AC (p<0.001), but no association was found with LSIL. Whereas Ki-67 expression showed highly significant association with LSIL (p=0.012), HSIL (p<0.001), SCC (p<0.001) and AC (p<0.001).
CONCLUSION: p53 expression progressively increased from normal cervical epithelium to intraepithelial lesion to malignant lesion. pRb expression showed shift of expression of pRb(n) in intraepithelial lesions to expression of pRb(c) in HSIL to frank malignancy. Ki-67 expression was directly proportional to the degree of dysplasia to malignant lesion.
Introduction
Carcinoma cervix is the fourth most common malignancy among the women worldwide with an estimated 5,28,000 new cases in 2012 and accounts for almost 12% of all female cancers. An estimated 2,66,000 deaths from cervical cancer worldwide in 2012 is documented, accounting for 7.5% of all female cancer deaths. In India, 1,23,000 new cases and 67,000 deaths documented because of cervical cancer in 2012 (Globacan, 2015). Cervical cancer accounts for 17.5%, in a study undertaken at Kolar, South-eastern Karnataka, India Kalyani R et al, 2010. Carcinoma cervix emerges from a defined series of preneoplastic lesions with increasing cellular dysplasia referred to as cervical intraepithelial neoplasia (CIN) grade I, II and III Bahnassy AA, 2007. Many epidemiological studies conducted over the last 20 years have established a strong association between the high risk human papilloma virus (HPV type 16 and 18) and cervical cancer in up to 95% of cases.
The important regulators disrupted in cervical cancer cells are two tumor suppressor genes, retinoblastoma protein (Rb) and p53 transcription factor. The interconnecting signaling pathways controlled by Rb and p53 are involved in the etiology of cervical cancer Sherr CJ, 2002.The Ki-67 protein plays an important role in cell proliferation. Its antigen is expressed during the cell cycle with the exception of the G0 phase, and has been used as a marker for proliferation in various tumors, including cervical carcinoma Mocuţa D, 2010.
Material and methods
In the present study 120 samples (cases & controls) were considered. Prior to the study ethical clearance was obtained from the institutional ethical board. Patients attending department of Obstetrics and Gynecology for cervical cancer screening as well as with complaints of white discharge per vagina, bleeding per vagina and mass per vagina were considered. Clinical data was obtained in each case regarding name, age, history of present illness, personal history and any other associated complaints.Consent from the patient was taken for local examination and biopsy was taken from the suspected area after application of 5% acetic acid or Lugol’s iodine. Hysterectomy specimens were also considered for the study. Biopsy was routinely processed and stained with Hematoxylin and Eosin staining. The sections were examined for dysplasia, carcinoma in situ and malignancy.
Immunohistochemistry (IHC) was performed on 3-μm thick sections from 10% formalin-fixed paraffinembedded tissues. Horse-peroxidase method was used for a panel of three antibodies i.e, p53 (Biogenex, BP53-12), Ki-67 (Biogenex, BGX-297) and pRb (Biotech, Rb(IF8)SC-102). For antigen retrieval, citrate buffer of pH-6.0 using microwave power 10 for 6 minutes x 3 cycles was done (applicable for all 3 antibodies). Counter stain done with Haematoxylin. All the slides were examined. To ensure the reliability of the experimental study, internal quality control of immunohistochemical techniques was performed as a part of an implemented and certified quality assurance system.
Cells were noted as positive when they showed nuclear/ cytoplasmic immunoreactivity (brown precipitate). Only the neoplastic region of each tissue section was evaluated. To evaluate the marker positivity, at least 1000 cells per case was counted. Quantification of the results was made by determining the nuclear positivity (number of cells marked by the antibody divided by the number of cells counted per sample). Positivity was nuclear for p53, Ki-67 and nuclear & cytoplasmic for pRb. The percentage of positive cells in each tissue section was estimated on a semiquantitative scale where: 0(0%), +1 (1-24%), +2 (25- 49%), +3 (50-74%), +4 (75-100%). The staining intensity was also assessed based on the category as mild, moderate and high or grade I to III. This is mainly based on subjective assessment. The mean values of IHC markers were correlated with different stages of the disease Greene FL, 2006.
The data was suitably arranged into tables. Descriptive statistical analysis was carried out on this data. Results on continuous measurements are presented as mean ± standard deviation and results on categorical measurements are presented in number%. Significance was assessed at 5% level of significance. The mean value of p53, pRb and Ki-67 was compared between normal and various premalignant and malignant lesions separately using Independent‘t’ test.
Results
Out of 120 samples, 20 were normal cervix, 21 low grade squamous intraepithelial lesion (LSIL), 18 high grade squamous intraepithelial lesion (HSIL), 13 well differentiated squamous cell carcinoma (WDSCC), 28 moderately differentiated squamous cell carcinoma (MDSCC), 7 poorly differentiated squamous cell carcinoma (PDSCC), 8 Non-keratinising squamous cell carcinoma (NKSCC), 3 adenocarcinoma (AC) and 1 each of Adenosquamous (AS) and microinvasive (MI) carcinoma respectively. Classification of the carcinoma was based on Modified World Health Organization criteria Ellenson LH, 2010. The age group ranged from 30-79 years, the highest malignancy was in the age group of 40-49yrs.
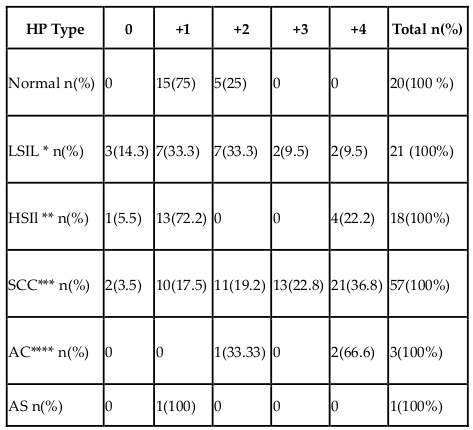
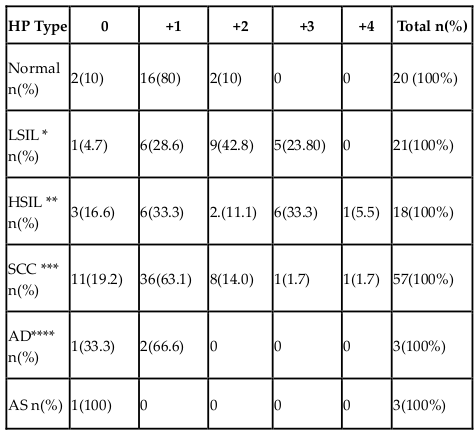
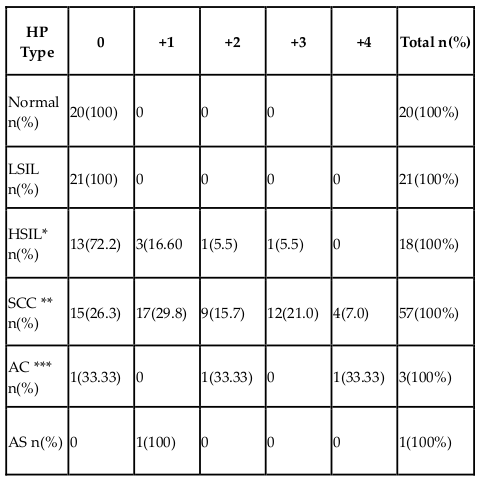
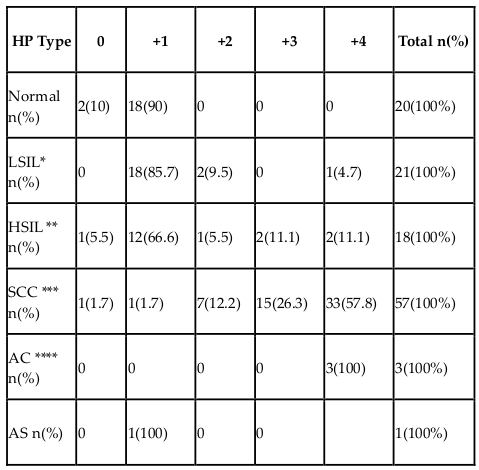
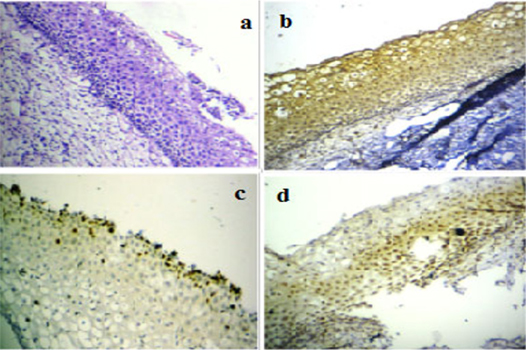
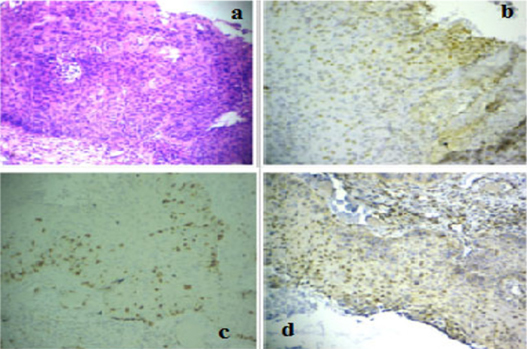
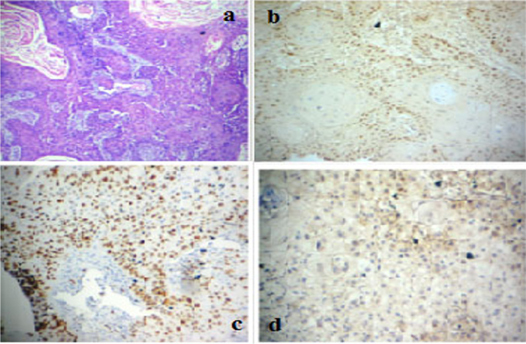
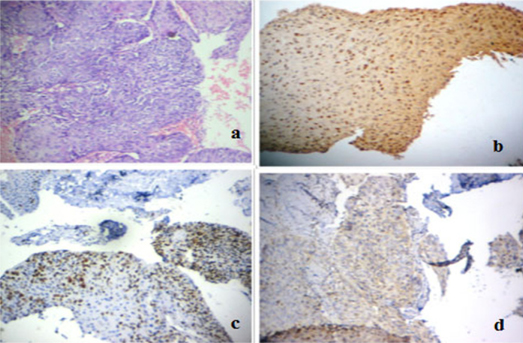
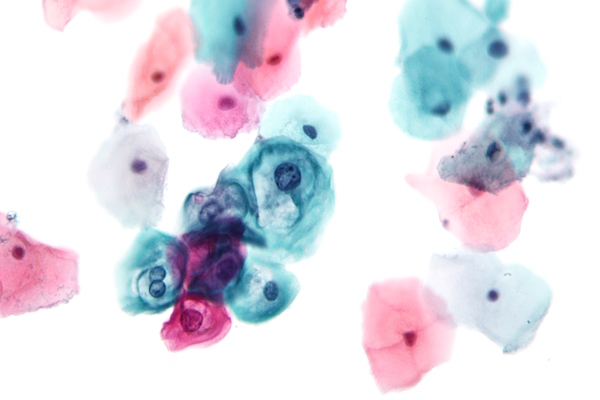
p53 immunoscoring in various lesions are shown in Table 1 . There was significant association of p53 expression between normal cervical epithelium and LSIL (p=0.023), SCC (p<0.001) and AC (p=0.004) but no significant association with HSIL (p=0.09).pRb(n) (n=nuclear) immunoscoring in various lesions are shown in Table 2 . pRb(n) expression showed significant association when normal was compared with LSIL (p<0.001) and HSIL (p=0.001), no association was found with SCC (p=0.207) and AC (p=0.322). pRb(c) (c=cytoplasmic) immunoscoring in various lesions are shown in Table 3 . pRb(c) expression showed significant association when normal was compared with HSIL (p=0.03), SCC (p<0.001) and AC (p<0.001), but no association was found with LSIL. Ki-67 immunoscoring in various lesions are shown in Table 4 . Ki-67 expression showed highly significant association with LSIL (p=0.012), HSIL (p<0.001), SCC (p<0.001) and AC (p<0.001) ( Figure 1 Figure 2 Figure 3 Figure 4 Figure 5 ).
Comparing IHC markers with intensity of staining and various lesions, regarding p53 majority of normal, pre-neoplastic lesions (LSIL, HSIL) and NKSCC was grade I;.KSCC (Keratinising squamous cell carcinoma) and AC was grade II/III. In pRb(n) marker, majority of normal, pre-neoplastic, KSCC and NKSCC was grade I. In pRB(c) marker, majority of normal, PDSCC and AC showed grade 0; NKSCC grade 0/I and KSCC grade I. In Ki-67 marker majority of normal was grade I; pre-neoplastic, MDSCC and PDSCC grade II; NKSCC Grade II/III; WDSCC and AC grade III. However there was no significant statistical correlation between intensity of staining of normal with various pathological lesions.
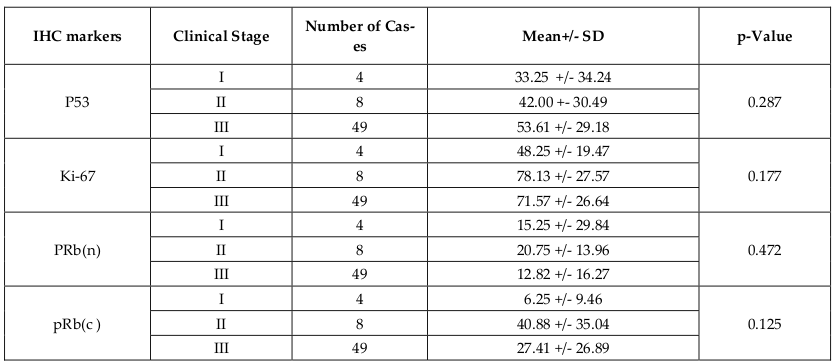
No statistical significant correlation was found comparing mean values of IHC markers and clinical staging of the disease ( Table 5 ).
Discussion
Cervical carcinoma is one of the most common malignancies affecting women Vasilescu F, 2009. HPV is known to be the most important cause of cervical cancer. High risk type (16, 18) viruses are implicated in the pathogenesis of cervical neoplasm which is induced by a multistep process. In addition, the progression of the cervical cancer can be influenced by the immune surveillance or other carcinogens Tommasino M, 2003. Low and/or high-grade cervical intraepithelial neoplasia (CIN) can regress or progress to an invasive cervical carcinoma after a long period of latency. The HPV genome encodes proteins that are able to induce unscheduled proliferation and prevent apoptosis Chakrabarti O, 2003.
The two early HPV genes, E6and E7, play crucial role in tumour formation. There is integration of viral DNA into host DNA which is the critical step in cervical carcinogenesis. E6 and E7 are the viral oncoproteins, uncontrolled expression of these proteins are seen when there is inactivation of host tumor suppressor genes (p53 &pRb). This will result in loss of normal maturation sequence, causing persistent, proliferative HPV infection. This will further result in transformation to high grade dysplasia and progresses to invasive carcinoma Kalof AN, 2007Magaldi TG, 2012. The multistep process of carcinogenesis is based directly or indirectly on cell proliferation. Ki-67 is a nuclear proliferation associated antigen and a well known cell proliferation marker Kim SM, 2001. Cell proliferation has been described as an additional parameter useful in the prognostic evaluation of cervical cancer Agnaldo LS, 2004Qiangxiu W, 2004. The current study was done to know the role of these biomarkers/ cellular proteins in various grades of dysplasia and malignancy.
In the present study, maximum cases of premalignant and malignant cervical lesions were found in the age group of 40-49 years. Maximum frequency of cases in older women beyond 40 years of age (SIL-10.71%, carcinoma cervix- 1.3%) is reported Misra JS, 2009. Another study reported similar age distribution Kalyani R, 2010. One study concluded that the most common age group involved in carcinoma cervix ranged from 35-50 year Aswathy S, 2012.
About 90% of cervical cancers are squamous cell carcinomas and rest 10% are adenocarcinoma. Around 85-90% of cases of squamous cell carcinoma and the rest adenocarcinoma are reported in various studies Das BC, 2000Misra JS, 2009. In another study majority of cervical carcinomas were histologically squamous cell carcinoma followed by adenocarcinoma Kalyani R, 2010.
P53, tumour suppressor gene, plays an important role in protection against the development of cancer. Wild type p53 monitors the integrity of the genome. The mechanism of activation of p53 in response to DNA damage depends on DNA protein kinase Levine AJ, 1991.The p53 gene is one of the most important targets of the HPV E6 gene. Two important mechanisms are known as to how p53 causes cervical cancer. The first, E6 binds to E6 associated protein (E6AP), which functions as ubiquitine protein ligase. E6/E6AP complex binds the central region of p53, which becomes rapidly ubiquitinated and is targeted to proteosomes. Thus E6 protein has the capacity to stimulate p53 degradation. This leads to low levels of p53 in cervical tumor cells. In conclusion, inactivation of p53 represents a key step in cervical carcinogenesis Levine AJ,1991Madhumita Roy, 2014Tan GC, 2007Tommasino M, 2003. Secondly, mutation of p53 is rarely found to cause carcinomas. However mutation can be found in both HPV positive or negative cervical tumours, indicating that there is no correlation between HPV and p53 status. Mutated p53 suggests that p53 can be functionally inactivated in cervical cancer cells either by association with E6 or mutation of the gene Tommasino M, 2003.
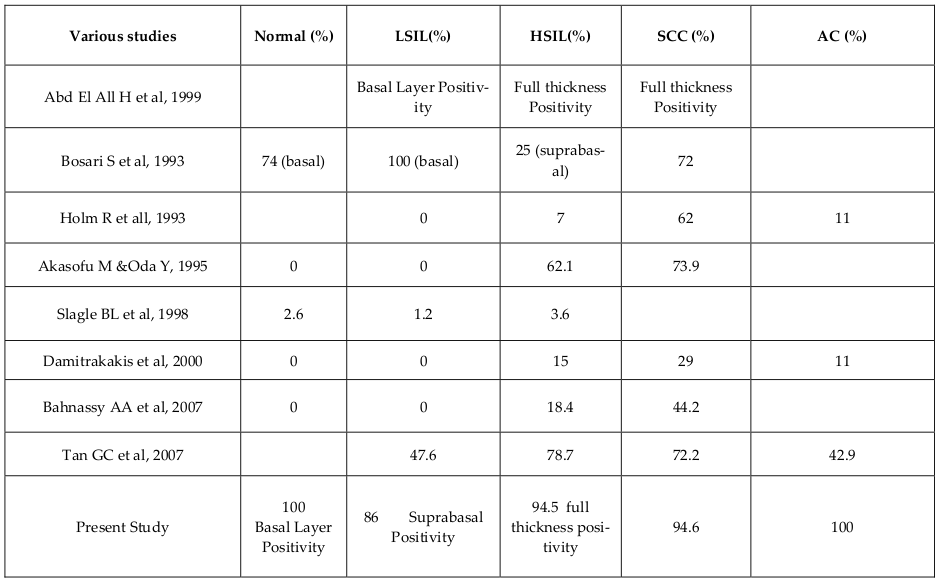
p53 immunoreactivity starts in SIL. The expression of p53 begin to be seen in a few cells in the basal layer of LSIL and increase in parallel to the extension of neoplastic cells in HSIL and carcinoma in situ and was more extensive in invasive lesions Abd El All H, 1999. The results of various studies are shown in Table 6 . In the present study, p53 was detected in all cases of normal cervical epithelium in the basal layer, of which 75% showed +1 score and 25% showed +2 scoring. Among premalignant lesions, 86% of LSIL cases showed positivity in basal and suprabasal region, out of which 33.3% of cases showed immunoreactivity with +1 and +2 scoring respectively. 94.4% of HSIL cases showed suprabasal/full thickness positivity, out of which 72.2% of cases showed +1 scoring, 22.2% cases showed +4 scoring. On the contrary, when LSIL cases were compared with normal cases, significant association was found (p=0.023). But this was not true in case of HSIL where no significant association was found. 94.6% of invasive squamous cell carcinoma showed p53 expression, out of which 35.7% showed +4 scoring. In comparison with normal cervical epithelium, significant association was found (p<0.001) (Table 1). Although the rates of p53 positivity in cervical carcinoma differ in different studies, all of them indicate that p53 immunoreactivity is commonly detected in invasive SCC. However another study showed that there are no statistical differences between the expression of p53 in SCC, CIN, squamous metaplasia and normal squamous mucosa Son SM, 2012.
Conflicting results on this topic have been published. Positive p53 immunoreactivity which was detected in normal cervical epithelium can be explained as a result of over expression or stabilization of the wild type, or as an effect of the microwave oven heating in the absence of mutations Tan GC, 2007. This could probably be the reason of over expression of p53 in normal cases in our study also. Some studies showed a significant correlation of p53 expression with HSIL compared with normal, whereas others showed no significant association Zamora PC, 2009.
The possible explanation for over expression of p53 in SCC may imply several things: p53 gene may be randomly mutated, abnormal accumulation of nonmutant p53 protein due to altered p53 homeostasis in tumour cells rather than p53 mutation, conformational changes in wild type p53 protein causing it to change from suppressor to promoter or mutant p53 and/or detected p53 may be normal p53 that is abnormally stabilised or increased in amount Zamora PC, 2009. The expression of p53 beyond the basal cells in intraepithelial lesions indicates loss of normal proliferation cell regulation and loss of epithelial maturation especially in HSIL Godoy AEG, 2014.
Adenocarcinoma and adenosquamous carcinoma has bad prognosis when compared to squamous cell carcinoma. Therefore p53 expression would be expected to be greater in the former two. In our study, p53 expression was found to be greater in adenocarcinoma. This finding does not reflect the true population as there was only 4 cases available for evaluation and association with normal does not carry much value even though it was found to be significant.
When the intensity of staining was evaluated in our study, both normal and premalignant cases showed grade I (mild) intensity. However malignant cases showed grade II to III (moderate to intense) intensity. In a study majority of CIN showed negative to grade I intensity, whereas 65.2% of malignant cases showed grade III intensity Galgano MT, 2010.
The protein product of the Rbgene (pRb; retinoblastoma protein) is a nuclear phosphoprotein that plays an important role in regulating the cell cycle. Therefore loss of normal Rb function may allow cells to proliferate in an uncontrolled manner, not only to initiate events in tumourigenesis, but also as a step associated with malignant progression Noraini MD, 2003.Loss of normal Rb function can be either due to mutation of Rb gene or binding of HPV-E7 to Rb-E2F which removes cell cycle restriction. HPV-16 E7 interacts with and functionally inactivates the tumour suppressor protein pRb. E7 also induces destabilization of the retinoblastoma protein. The resulting release of active E2F transcription factors leads to stimulation of Sphase cell cycle entry. E7 protein is found predominantly in the nucleus and to a minor extent in the cytoplasm in the cervical cancer cell line Ca Ski in vitro and in cervical carcinoma in situ, suggesting that nuclear resident E7 plays a major role in cervical carcinogenesis in humans Fiedlwer M, 2004Hui-Min Chen, 2014Madhumita Roy, 2014 .The majority of Rb mutations lead to absence of Rb mRNA and its protein product. The complete absence of nuclear reactivity in all areas of tumour associated with a positive internal control has shown a strong indication of underlying Rb mutations Noraini MD, 2003.
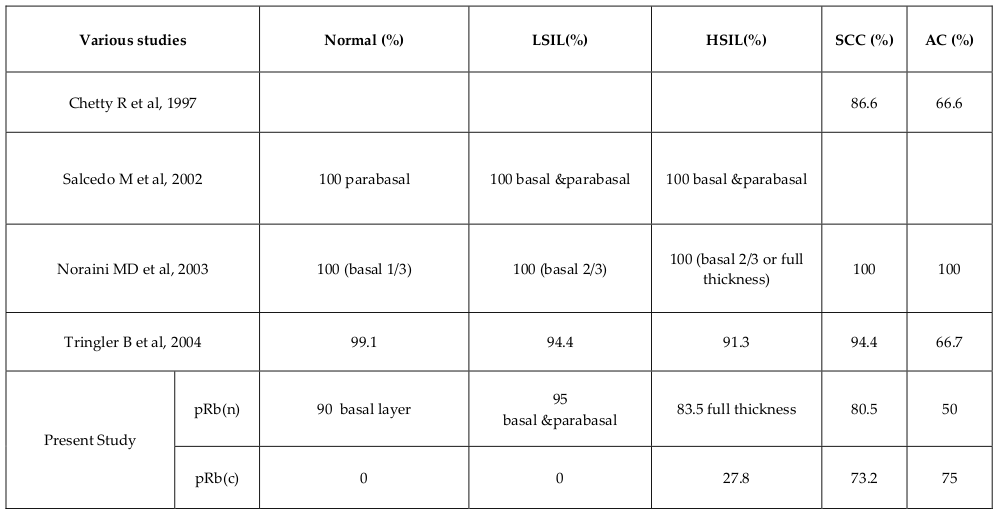
Higher pRb expressions in premalignant lesions were observed when compared to normal cervical epithelium Amortegui AJ, 1995. Table 7 shows the results of various studies.pRb staining was lower in invasive carcinoma than SIL, suggesting that Rb gene down regulation could be involved in cervical carcinogenesis Salcedo M, 2002. Majority in normal cervical epithelium showed +2 score and premalignant cases +3 score Noraini MD, 2003. Loss or reduction of pRb expression in aggressive behavior of breast cancer is reported Ceccarelli C, 1998. In our study, pRb(n) immunoreactivity was seen in 90% of normal cervical epithelium in basal layer, of which 80% showed +1 score. In case of premalignant lesions, 95% of LSIL cases showed positive immunoreactivity in basal and parabasal layer, majority of which showed +2 score. 83.5% of HSIL cases showed positivity in basal ¶basal layer/full thickness with majority showing +1 & +3 score. One more finding which we would like to highlight here is the appearance of cytoplasmic stain in HSIL (27.8%) cases. When pRb(n) immunoscoring was compared between normal cervical epithelium and LSIL, significant association was found (p<0.001). But no association was found for pRb(c). We also found significant association between normal cervical epithelium and HSIL cases for both pRb(n)(p=0.001) and pRb(c)(p=0.03) ( Table 2 Table 3 ). 80% of malignant lesions showed positive pRb(n) immunoreactivity, out of which, 64% showed +1 score, 12.5% showed +2 score, 1.8% each showed +3 and +4 respectively. 20% of cases showed no staining. The percentage of immunoreactivity in case of PDSCC is low when compared to WDSCC & MDSCC. PDSCC showed 0 to +1 score when compared with WDSCC & MDSCC which showed +1 to +2 score. The percentage of pRb positive cells was higher in SIL than in normal cervical epithelium which may be due to increased proportion of proliferating cells. This is supported by the fact that hyperphosphorylatedpRb is increased during G2/M phases Bosari S, 1993Noraini MD, 2003. One study showed that pRb expression was relatively less in CIN II/III and SCC compared to normal squamous epithelium and squamous metaplasia Son SM, 2012.
In case of pRb(c) immunoreactivity, 73% of malignant lesions showed positivity, out of which 28.6% of cases showed +1 score, 16% of cases showed +2 score, 21.4% showed +3 score and 7.2% showed +4 score. 27% of cases showed no staining. When pRb(n) immunoscoring was compared between normal and invasive squamous cell carcinoma, no significant association was found, whereas for pRb(c), significant association was found (p<0.001) ( Table 2 Table 3 ).
In case of adenocarcinoma, out of 3 cases, 2 of them showed +1 scoring. Since the number of cases was very less, commenting on its immunoreactivity was not possible. An additional finding was the presence of cytoplasmic staining, which appeared in HSIL and increased in proportion in WDSCC and MDSCC, but decreased in PDSCC. This finding has been observed in many other studies but the reason is still not known. It was thought to be an artifact by some investigators or it could be related to Rb gene mutation Salcedo M,2002.One more reason could be the dispersion of gene products from the nucleus to the cytoplasm which will take up the brown stain. Studies have shown that E7 protein was found predominantly in the nucleus and to a minor extent in the cytoplasm in cervical carcinoma. The oncoprotein in HPV, E7, binds with Rb and forms a complex which could be present in the cytoplasm that will also take up the stain. Further studies should be done to support these finding. Cytoplasmic immunoreactivity in mitotic cells indicates that in the absence of nuclear envelope, pRb diffuses to other cellular locations Salcedo M, 2002.
The staining intensity of pRb(n) varies from grade 1 to 2 in both premalignant and malignant lesions, whereas for pRb(c) it varies from grade 0 to 1. This variation in staining probably resulted from asynchronous progression of the cells through the cell cycle.
Ki67 is a cell cycle associated protein present in the peri-chromosomal region, expression of which is associated with cell proliferation to measure growth fraction of cells in human tumors. Ki67 nuclear antigen is a non-histone heterodimer that is detected in nuclei of cells during G1, S, G2 and mitotic phase of the cycle. Ki67 is the gold standard proliferative index and is immunhistochemically detectable throughout the interphase of the cell cycle, reaching its maximal level during mitosis. Immediately after mitosis, the cellular Ki67 antigen content decreases due to the short half life and is not detectable in Go phase Carreras R,2007.
Table 8 shows results of ki-67 marker in various studies. Invasive squamous cell carcinoma is reported to have +2 to +4 score Agnaldo LS, 2004. Ki-67 expression is useful in distinguishing the different grades of dysplasia, though not predicting their behavior Carreras R, 2007. One study showed that invasive carcinoma (SCC & AC) has +4 score which indicates that Ki-67 expression has a tendency to correlate positively with the histologic grade Zamora PC, 2009. Ki-67 expression is greater in CIN samples than in normal/metaplastic epithelium and Ki-67 staining is stronger in high-grade CIN than in low-grade CIN. Therefore, Ki-67 is usually used to differentiate and grade CIN Godoy AEG, 2014Kim SM, 2001. One study has shown increased expression of Ki-67 in SCC, CIN I/II/III but negative expression in squamous metaplasia and normal squamous mucosa Son SM, 2012. However Ki-67 cannot be used to differentiate between HPV induced dysplasia and benign proliferating cells due to benign reactive process Hwang SJ, 2012. In our study, 90% of normal cases showed positivity for Ki-67 only in the basal layer, that is, +1 score. All the LSIL (100%) cases showed Ki-67 positivity in basal and suprabasal layer, out of which majority (85.7%) showed +1 score, but a few cases (5%) showed higher expression. In case of HSIL, 94.5% of cases showed Ki-67 expression (full thickness), of which 66% of cases showed +1 score and 11% of cases showed +4 score. The expression of Ki-67 was significantly higher in invasive squamous cell carcinoma cases, 98.2%, out of which 60% had +4 score. We also found a significant association when compared with normal cervical epithelium (p<0.001). This finding shows that Ki-67 expression correlates with the histological grade of cervical neoplasia. We also found that all adenocarcinoma cases showed Ki-67 positivity with +4 scoring. A significant association was found between normal cervical epithelium and adenocarcinoma cases as well (p<0.001) ( Table 4 ). Since the number of cases was very less, commenting on its results has less value.
However there is various contradicting opinion where one study states that the study failed to identify the significant correlation between the markers which regulates the mitotic cycle as p53, pRb and Ki-67 to the course of LSIL Quint KD, 2013. The markers when used in combination also helps to grade the dysplasia as seen in a study where p53(-)Ki-67(+)bcl2(-) was commonly seen in HSIL and p53(-)Ki-67(-)bcl2(-) in LSIL and normal epithelium Godoy AEG, 2014. The combination of E6 with p53 and E7 with pRb is also studied where the LSIL and HSIL showed integration of E6 and E7 in almost all cases with absent interaction of E6/p53 and E7/pRb Benedetto GD, 2014
An attempt to grade the intensity of staining was made in this study, which showed that normal cervical epithelium cases (13 out of 20) showed mild (grade I) staining. In premalignant lesions, moderate (grade II) staining was noted. In case of invasive carcinomas, the intensity ranges from grade II – III.
An effort was also made to know if there was any significant association between the markers and clinical stages. Unfortunately, no significant association was found between them. One study showed that there was no correlation of p53 expression with tumour size, histologic grade, depth of invasion and lymphovascular space invasion in early stage cervical carcinomas Khunamornpong S, 2008.
Conclusion
Squamous cell carcinoma of cervix is commonly seen in 4th to 5th decade of life. P53 expression progressively increased from normal cervical epithelium to intraepithelial lesion to malignant lesion. However pRb (n) expression was maximum in intraepithelial lesion compared to normal cervical epithelium and malignant lesion. pRb(c) expression as p53 protein progressively increased from intraepithelial lesion to frank malignancy. Ki-67 expression was directly proportional to the degree of dysplasia to malignant lesion. However further studies is required to exactly analyze the cytogenetic aberration in p53 and pRb genes. The present study can be used as a base line study of the expression of p53 and pRb protein in cervical neoplasia.
References
-
GLOBOCAN Cancer Fact Sheets: Cervical Cancer. [homepage on internet] (Available from globocan.iarc.fr/old/FactSheets/Cancer/Cervixnew. asp ).
.
-
R.A.
Abd El All H,
P
Duvillard.
p53 Immunohistochemical expression of Egyptian cervical carcinoma. PatholOncol Res.
1999;
5(4)
:
280-284
.
-
P.T.
Agnaldo LS,
AT
Sergio.
Expression of p53, Ki-67 and CD 31 in the vaginal margins of radical hysterectomy in patients with stage IB carcinoma of the cervix. Gynecoloncol.
2004;
95(3)
:
646-654
.
-
M.M.
Amortegui AJ,
VL
Elborne,
RM
Amin.
P53, retinoblastoma gene product and cyclin protein expression in human papillomavirus DNA-positive cervical intraepithelial neoplasia and invasive cancer. Mod Pathol.
1995;
8(9)
:
907-912
.
-
Q.M.
Aswathy S,
B
Kurian,
K
Leelamoni.
Cervical cancer screening: Current knowledge & practice among women in a rural population of Kerala, India. Indian J Med Res.
2012;
136(2)
:
205-210
.
-
Z.A.
Bahnassy AA,
M
Saleh.
The possible role of cell cycle regulators in multistep process of HPV-associated cervical carcinoma. BMC ClinPathol.
2007;
7
:
4
.
-
M.V.
Benedetto GD.
The detection of complexed proteins E6/P53 and E7/Prb in relation to carcinogenesis of uterine cervix. J CytolHistolS4: 022doi:10.4172/2157-7099.
2014;
S4022
.
-
R.M.
Bosari S,
G
Viale.
p53immunoreactivity in inflammatory and neoplastic diseases of the uterine cervix. J.
1993;
Pathol169(4)
:
425-430
.
-
A.F.
Carreras R,
G
Mancebo.
A study of Ki-67, c-erbB2 and cyclin D-1 expression in CIN-I, CIN-III and squamous cell carcinoma of the cervix. HistolHistopathol.
2007;
22(6)
:
587-592
.
-
S.D.
Ceccarelli C,
P
Cheicom.
Retinoblastoma (RB1) gene product expression in breast carcinoma. Correlation with Ki-67 growth fraction and biopathological profile. J ClinPathol.
1998;
51(11)
:
818-824
.
-
K.S.
Chakrabarti O.
Molecular interactions of ‘high risk’ human papillomaviruses E6 and E7 oncoproteins: Implications for tumour progression. J Biosci.
2003;
28(3)
:
337-348
.
-
G.V.
Das BC,
S
Hedau,
S
Katiyar.
Cancer of uterine cervix and Human Papilloma Virus infection. Current Science.
2000;
78(1)
:
52-56
.
-
P.E.
Ellenson LH.
The Female Genital Tract. In: Kumar V, Abbas AK, Fausto N editors. Robbins and Cotran pathologic basis of disease. 8th edition. NewDelhi: Saunders Elsevier.
2010;
:
1017-1024
.
-
M.-H.E.
Fiedlwer M,
HP
Viertler.
High level HPV-16 E7 oncoprotein expression correlates with reduced pRb levels in cervical biopsies. FASEB J.
2004;
18(10)
:
1120-1122
.
-
C.P.
Galgano MT,
KA
Atkins.
Using biomarkers as objective standards in the diagnosis of cervical biopsies. Am J.
2010;
SurgPathol34(8)
:
1077-1087
.
-
B.K.
Godoy AEG,
LBD
Moura,
EP
Serafini.
Expression analysis of p53, Ki-67 and bcl2 in premalignant lesions of cervix. Journal of Obstetrics and Gynecology.
2014;
4
:
462-469
.
-
C.C.
Greene FL,
AG
Fritz.
AJCC Cancer Staging Atlas, 6th edn. Chicago: Springer.
2006
.
-
Chen D.-G.Z.J.-X.W.D.-S.P.J.-N.Z.
Hui-Min.
Ubiquitination of p53 is Involved in Troglitazone Induced Apoptosis in Cervical Cancer Cells. Asian Pacific Journal of Cancer Prevention.
2014;
15(5)
:
2313-2318
.
-
S.K.
Hwang SJ.
Biomarkers of cervical dysplasia and carcinoma. Journal of Oncology.
2012;
2012
:
507286
.
-
C.K.
Kalof AN.
Our approach to squamous intraepithelial lesions of the uterine cervix. J ClinPathol.
2007;
60(5)
:
449-455
.
-
D.S.
Kalyani R,
Kumar H
Bindra Singh MS.
Cancer profile in the Department of Pathology of Sri DevarajUrs Medical College Kolar: A ten years study. Indian J Cancer.
2010;
47(2)
:
160-165
.
-
S.S.
Khunamornpong S,
S
Manusirivithaya.
Prognostic value of p53 expression in early stage cervical carcinoma treated by surgery. Asian Pacific J of Cancer Prev.
2008;
9(1)
:
48-52
.
-
L.J.
Kim SM,
DW
Lee,
MJ
Kim,
HN
Lee.
The Prognostic Significance of P16, Ki-67, P63, and Ck17 Expression Determined By Immunohistochemical Staining in Cervical Intraepithelial Neoplasia. Korean J ObstetGynecol.
2001;
54(4)
:
184-191
.
-
M.J.
Levine AJ,
CA
Finlay.
The p53 tumour suppressor gene. Nature.
1991;
351(6326)
:
453-456
.
-
S.M.
Madhumita Roy.
Reversal of Resistance towards Cisplatin by Curcumin in Cervical Cancer Cells. Asian Pacific Journal of Cancer prevention.
2014;
15(3)
:
1403-1410
.
-
A.L.
Magaldi TG,
S
Bellone.
Primary human cervical carcinoma cells require human papillomavirus E6 and E7 expression for ongoing proliferation. Virology.
2012;
422
:
114-124
.
-
S.S.
Misra JS,
U
Singh,
AN
Srivastava.
Risk-factors and strategies for control of carcinoma cervix in India: Hospital based cytological screening experience of 35 years. Indian J Cancer.
2009;
46(2)
:
155-159
.
-
P.T.
Mocuţa D,
T
Szasz,
E
Lazăr.
Precancerous Cervical Lesions and Immunomarkers for Their Prognosis. StudiaUniversitatis.
2010;
20
:
87-93
.
-
S.-A.M.
Noraini MD,
SW
Kwan.
An Immunohistochemical study of retinoblastoma Gene product in normal, premalignant and malignant tissues of the uterine cervix. Malays J Med Sci.
2003;
10(1)
:
52-59
.
-
E.E.
Qiangxiu W,
C
Lihua,
W
Jiayao.
Expression of p53, Ki-67 and bcl-2 oncoproteins in human breast cancer and their clinicopathologic significance. Austral- Asian J cancer.
2004;
3
:
215-220
.
-
d.K.M.
Quint KD,
WGV
Quint,
EC
Pirog.
Progression of cervical low grade squamous intraepithelial lesion: in search of prognostic biomarkers. European Journal of Obstretic & Gynecology and Reproductive Medicine.
2013;
170
:
501-506
.
-
T.L.
Salcedo M,
D
Utrera.
Changes In retinoblastoma gene expression during cervical cancer progression. Int J.
2002;
ExpPathol83(6)
:
275-286
.
-
M.F.
Sherr CJ.
The Rb and P53 Pathways in Cancer. Cancer Cell.
2002;
2
:
103-112
.
-
N.K.
Son SM,
HC
Lee,
YJ
Park,
EH
Jeong,
HS
Kim,
HG
Song.
Evaluation of p16INk4a, pRb, p53 and Ki-67 expression in cervical squamous neoplasia. J Biomed Res.
2012;
13(3)
:
209-217
.
-
S.N.
Tan GC,
S
Salwati,
MS
Shiran,
AZ
Hatta.
Immunohistochemical Study of p53 Expression in Premalignant and Malignant Cervical Neoplasms. Med & Health.
2007;
2(2)
:
125-132
.
-
A.N.
Tommasino M,
S
Caldeira.
The Role of TP53 in Cervical Carcinogenesis. Hum.
2003;
Mutat21(3)
:
307-312
.
-
C.M.
Vasilescu F,
C
Tănase.
P53, P63 and Ki-67 Assessment in HPV Induced Cervical Neoplasia. Rom J.
2009;
MorpholEmbryol50(3)
:
357-361
.
-
P.A.
Zamora PC,
FJO
Casado.
Effect of Human Papillomavirus on Cell Cycle-Related Proteins p16, Ki-67, Cyclin D1, p53, and ProEx C in Precursor Lesions of Cervical Carcinoma. A Tissue Microarray Study. Am J ClinPathol.
2009;
132
:
378-390
.
Comments
Downloads
Article Details
Volume & Issue : Vol 2 No 10 (2015)
Page No.: 374-384
Published on: 2015-10-29
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 7474 times
- Download PDF downloaded - 1764 times
- View Article downloaded - 5 times
 Biomedpress
Biomedpress