Abstract
Introduction: Many recent guidelines have highlighted the importance of genetic factors in chronic obstructive pulmonary disease (COPD) development. Adrenoreceptor beta 2 (ADRB2) is believed to be linked to the response to beta 2 agonists. However, the data for this gene remains controversial. In our study we aimed to investigate the impact of the Gln27Glu gene polymorphism of ADRB2 on the clinical course of COPD.
Methods: 100 patients were included into the study. We assessed GOLD group, number of exacerbations, hospitalizations, modified Medical Research Council (mMRC) dyspnea and COPD assessment test (CAT) scores, and the utilization of antibiotics, glucocorticoids, and xanthines in these patients, as well as genetic testing at inclusion. All patients had their medication changed to tiotropium/olodaterol.
Results: Groups did not differ according to age, sex, smoking status, pack-years, or COPD duration. We found that patients with the Gln27Gln polymorphism had the lowest GOLD grading, D. No difference was found in the number of exacerbations, hospitalizations, and out-patient exacerbations in the year prior to inclusion and the study year. Tiotropium/olodaterol were comparable in all study groups in reducing exacerbations and hospitalizations. There was no significant difference in mMRC and CAT values between the groups. We found that Gln27Gln patients required less antibiotics at inclusion and less glucocorticoids at the end of the study. Tiotrpium/olodaterol showed variable results for different genotypes regarding the reduction in use of different drugs.
Conclusion: This ADRB2 polymorphism was associated with the progression of COPD as it is linked to a more severe phenotype, requiring greater use of antibiotics and glucocorticoids. This indicates potential crosstalk at the cellular level between ADRB2 and glucocorticoid receptors and should be investigated further.
Introduction
Chronic obstructive pulmonary disease (COPD) is a widespread and treatable disease. It is characterized by persistent symptoms of pulmonary function decline secondary to changes in the airways and/or alveoli, usually caused or triggered by environmental factors, such as tobacco smoke, on the susceptible organism1. Data collected in the BOLD (Burden of Obstructive Lung Disease) study states that COPD affects 10.1% of people globally, with higher prevalence in men (11.8%) compared to women (8.5%)2. Several studies have also shown a high prevalence of COPD in never smokers (3 — 11%)2, 3. Blanco et al. measured COPD prevalence in Europe to be 12.4%4, and it accounts for more than 3 million deaths annually, worldwide5. Some studies also predict that COPD will be the cause of 5.4 million deaths by the year 2060 due to the wider spread of smoking in developing countries, and ageing populations in developed countries6. COPD also severely increases the risk of co-morbidities, including those from the top ten leading causes of death, such as coronary artery disease, strokes, diabetes mellitus type 2, chronic kidney disease, pneumonia, and lung cancer7, 8, 9, 10.
As has been stated in guidelines, COPD development requires a combination of environmental and internal factors, and multiple studies have suggested an important role for several genes related to the regulation of inflammation, fibrosis, and airway responsiveness11. One of these is adrenoreceptor beta 2 (ADRB2), which some studies have shown to be related to COPD development12, severity13, and response to beta-2 agonists14. One study showed varying prevalence of ADRB2 gene alleles in COPD patients and healthy controls15 and there is also data suggesting that ADRB2 polymorphisms are related to the response to inhaled corticosteroids16, 17. In our study we aimed to investigate the impact of the Gln27Glu polymorphism of ADRB2 on the clinical course of COPD.
Methods
This study was performed at the Department of Propedeutics of Internal Medicine of the Vinnytsia National Pirogov Memorial Medical University and Vinnytsia City Clinical Hospital № 1. Local ethics committee permission was obtained prior to the start of the study. All patients signed informed consent prior to any study-related procedures.
100 patients with the diagnosis of COPD were included into the study average age was 64.09 ± 1.94 years. There were 66 men (66%) and 34 women (34%). There were 68 smokers or ex-smokers (68%) and 32 (32%) never smokers average smoking experience was 24.44 ± 4.84 pack-years. Average COPD duration was 9.35 ± 2.42 years.
The following inclusion criteria were used: age from 18 to 80 years; COPD diagnosis of at least 12 months prior to inclusion, proven by medical records of the patients or positive medical history; FEV1/FVC < 0.7 at inclusion. The following exclusion criteria were used: any relevant disease, laboratory disorder, or other relevant history that could affect patient safety during participation in this study inability of the patient to follow study procedures alcohol or illicit drug abuse in the medical history or at inclusion.
We performed 3 different visits during the study which comprised the following: visit 1 — baseline visit, visit 2 — study visit at 5 ± 1 weeks, visit 3 — final visit at 52 ± 1 weeks.
At the baseline visit all patients signed an informed consent form. We collected relevant medical records and checked inclusion criteria. We recorded data relevant to the purpose of the study which included: exacerbations in the previous 12 months, which were recorded separately as in-patient and out-patient exacerbations; smoking status and number of pack-years; COPD duration. Based on the medical records and information provided by the patient, we recorded data for previous use of the following drug groups: antibiotics (AB), glucocorticoids (GCS), and xanthines. For each of the drug groups, we recorded the reason for their use, number of separate courses, and total treatment duration in days. All patients completed a modified Medical Research Council (mMRC) scale and COPD Assessment Tool (CAT) questionnaire. Genetic testing was performed at visit 1 for the assessment of the Arginine-16-Glycine (Arg16Gly) polymorphism, also known as (+46A > G; rs1042713). For the study purposes all patients were switched to a combination of long-acting muscarinic antagonists (LAMA) and long-acting beta-agonists (LABA). All patients were taught to use the new inhaler properly.
At visit 2 we collected intermittent data for mMRC scale and CAT evaluation and reassured proper inhaler use. At visit 3 we collected the following information: exacerbations in the previous 12 months, which were separately recorded as in-patient and out-patient exacerbations; use of AB, GCS, and xanthines. For each of the drug groups, we recorded the reason for their use, number of separate courses, and total treatment duration in days. All patients completed mMRC scale and CAT questionnaires.
Genetic testing was performed using real-time polymerase chain-reaction at the laboratory of Vinnytsia National Pirogov Memorial Medical University. According to the genetic testing results, patients were divided into 3 groups: Arg16Arg (group 1) — 23 patients (23 %), Arg16Gly (group 2) — 39 patients (39 %), Gly16Gly (group 3) — 38 patients (38 %).
Statistical analysis was performed using SPSS (Version 26.0 for Windows; USA). Descriptive statistics were determined for each interval parameter and are represented by the mean value ± standard deviation (SD). We used the Kolmogorov Smirnov test for assessment of data distribution in the sample. Chi-square method was used to compare nominal values. Mann-Whitney U-test and T-test were used for the comparison of two independent samples with abnormal and normal data distribution, respectively. Wilcoxon test was used to compare two dependent samples with abnormal data distribution, and t-test was used to compare paired samples with normal data distribution. Three or more independent samples were analyzed by Kruskal-Wallis test. For correlation analysis we used Spearman correlation coefficient for abnormally distributed data and Pearson correlation coefficient for normally distributed data. Linear regression analysis was used to determine predictors of dependent variables. In regression analysis we only included data that had weak, moderate, strong, or very strong correlations with the dependent variable. Regression analysis results are presented in odds ratio [OR], 95% C. A significance of p < 0.05 was considered statistically significant.
| Group | Gln27Gln (n = 35) | Gln27Glu (n = 39) | Glu27Glu (n = 26) | p | |||
|---|---|---|---|---|---|---|---|
| Parameter | n | % | n | % | n | % | |
| Men | 21 | 60 | 29 | 74.4 | 16 | 61.5 | 0.367 |
| Women | 14 | 40 | 10 | 25.6 | 10 | 28.5 | 0.367 |
| Smokers | 24 | 68.6 | 28 | 71.8 | 16 | 61.5 | 0.683 |
| Study group | GOLD COPD | |||||
| B | C | D | ||||
| n | % | n | % | n | % | |
| Gln27Gln (n = 35) | 9 | 25.7 | 20 | 57.2 | 6 | 17.1 |
| Gln27Glu (n = 39) | 7 | 20 | 9 | 23.1 | 23 | 58.9 |
| Glu27Glu (n = 26) | 3 | 11.5 | 13 | 50 | 10 | 38.5 |
| χ2 | 15.526 | |||||
| р | p = 0.004 | |||||
| Groups | Gln27Gln | Gln27Glu (n = 39) | Glu27Glu (n = 26) | p |
|---|---|---|---|---|
| Parameter | ||||
| Age, years | 61.57 ± 1.76 | 64.69 ± 1.56 | 66.58 ± 1.68 | 0.127 |
| COPD duration ,years | 13.49 ± 2.16 | 9.69 ± 0.85 | 10.00 ± 1.06 | 0.136 |
| Pack-years | 23.60 ± 4.2 | 27.59 ± 3.75 | 20.85 ± 5.02 | 0.408 |
| Exacerbation 1 st year, n | 2.54 ± 0.276 | 2.77 ± 0.25 | 2.96 ± 0.27 | 0.320 |
| -Hospitalizations 1 st year, | 1.03 ± 0.15 | 1.33 ± 0.17 | 1.31 ± 0.23 | 0.448 |
| -Out-patient 1 st year, | 1.51 ± 0,202 | 1.46 ± 0.19 | 1.65 ± 0.12 | 0.243 |
| Exacerbations 2 nd years, | 1.51 ± 0.14 | 1.69 ± 0.2 | 1.81 ± 0.21 | 0.628 |
| -Hospitalizations 2 nd year, | 0.31 ± 0.01 | 0.36 ± 0.09 | 0.46 ± 0.13 | 0.583 |
| -Out-patient 2 nd year, | 1.23 ± 0.12 | 1.33 ± 0.19 | 1.35 ± 0.17 | 0.934 |
| Groups | Gln27Gln (n = 35) | Gln27Glu (n = 39) | Glu27Glu (n = 26) | p |
|---|---|---|---|---|
| Parameter | ||||
| mMRC1 | 2.31 ± 0.11 | 2.49 ± 0.1 | 2.54 ± 0.14 | 0.274 |
| mMRC2 | 2.17 ± 0.1 | 2.26 ± 0.09 | 2.27 ± 0.13 | 0.760 |
| mMRC3 | 1.89 ± 0.13 | 2.03 ± 0.12 | 2.00 ± 0.12 | 0.808 |
| CAT1 | 23.09 ± 1.35 | 25.49 ± 1.38 | 23.35 ± 0.14 | 0.315 |
| CAT2 | 18.8 ± 1.22 | 20.53 ± 1.32 | 18.92 ± 1.17 | 0.530 |
| CAT3 | 16.43 ± 1.33 | 17.42 ± 1.37 | 15.88 ± 1.23 | 0.854 |
| Group | Drugs | |||||
| AB | GCS | Xanthines | ||||
| n | % | n | % | n | % | |
| Gln27Gln (n = 35) | 29 | 82.9 | 16 | 45.7 | 14 | 40 |
| Gln27Glu (n = 39) | 39 | 100 | 26 | 66.7 | 18 | 46.2 |
| Glu27Glu (n = 26) | 24 | 92.3 | 14 | 53.8 | 8 | 30.8 |
| χ 2 | 7.370 | 3.353 | 1.538 | |||
| р | p = 0.025 | р = 0.187 | р = 0.463 | |||
| Groups | Gln27Gln (n = 35) | Gln27Glu (n = 39) | Glu27Glu (n = 26) | p |
|---|---|---|---|---|
| Parameter | ||||
| AB courses, n | 1.37 ± 0.16 | 1.59 ± 0.14 | 2.00 ± 0.22 | 0.052 |
| AB duration, n | 10.89 ± 1.33 | 12.15 ± 1.18 | 14.19 ± 1.66 | 0.235 |
| GCS courses, n | 0.89 ± 0.25 | 1.33 ± 0.46 | 0.73 ± 0.15 | 0.398 |
| GCS duration, n | 3.60 ± 0.81 | 5.46 ± 1.03 | 3.65 ± 0.76 | 0.341 |
| Xanthines coruses, n | 0.63 ± 0.18 | 1.23 ± 0.57 | 0.42 ± 0.14 | 0.407 |
| Xanthines duration, n | 3.46 ± 0.95 | 4.41 ± 1.1 | 2.23 ± 0.72 | 0.413 |
| Group | Drugs | |||||
| AB | AB | |||||
| n | % | n | % | n | % | |
| Gln27Gln (n = 35) | 22 | 44 | 7 | 20 | 8 | 22.9 |
| Gln27Glu (n = 39) | 29 | 74.4 | 15 | 38.5 | 15 | 38.5 |
| Glu27Glu (n = 26) | 20 | 76.9 | 14 | 53.8 | 9 | 34.6 |
| χ 2 | 1.784 | 7.585 | 2.175 | |||
| р | p = 0.410 | р = 0.023 | р = 0.337 | |||
| Groups | Gln27Gln (n = 35) | Gln27Glu (n = 39) | Glu27Glu (n = 26) | p |
|---|---|---|---|---|
| Parameter | ||||
| AB courses, n | 0.77 ± 0.12 | 1.03 ± 0.14 | 1.35 ± 0.18 | 0.034 |
| AB duration, n | 5.77 ± 1,0 | 6.59 ± 0,93 | 8.62 ± 1.25 | 0.124 |
| GCS courses, n | 0.23 ± 0.08 | 1.44 ± 1.02 | 0.69 ± 0.14 | 0.019 |
| GCS duration, n | 0.97 ±0.36 | 2.97 ± 1.08 | 3.38 ± 0.74 | 0.014 |
| Xanthines coruses, n | 0.29 ± 0.11 | 1.15 ± 0.76 | 0.38 ± 0.11 | 0.346 |
| Xanthines duration, n | 1.09 ± 0.36 | 2.90 ± 0.98 | 1.85 ± 0.57 | 0.250 |
Results
There were 21 (60%) men and 14 (40%) women in the Gln27Gln group, 29 (74.4%) men and 10 (25.6%) women in the Gln27Glu group, and 16 (61.5%) men and 10 (28.5%) women in Glu27Glu group, which was not significantly different (р = 0.367). Groups also did not differ by the number of smokers (р = 0.683) (Table 1).
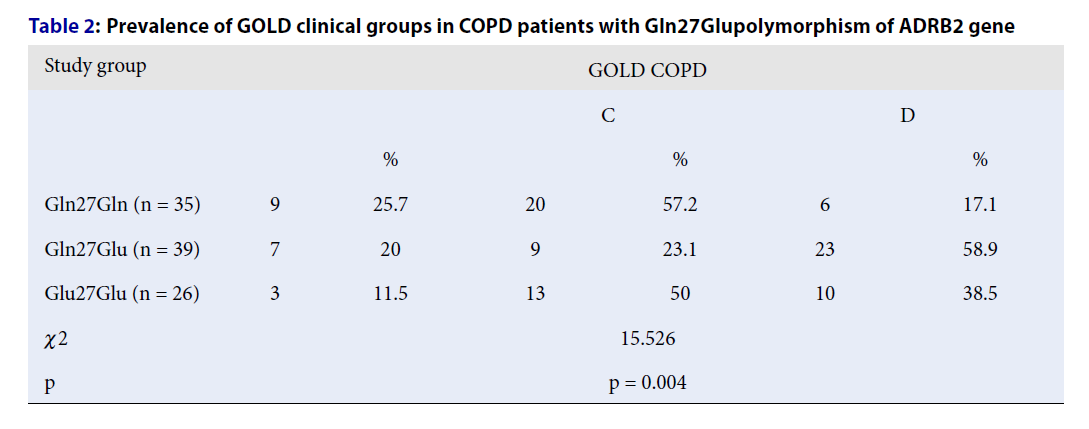
When the prevalence of GOLD groups was assessed using the chi-square method, there was a significant difference between the study groups (χ2 = 15.526, р = 0.004). There were no GOLD A group patients in the study, and there was a marked difference for group D patients, which consisted of 6 (17.5%) patients with Gln27Gln, 23 (58.9%) with Gln27Glu, and 10 (38.5%) in the Glu27Glu group (Table 2). There was a weak positive correlation between the Gln27Gln genotype with GOLD group C (r = 0.225, p = 0.024) and a weak negative correlation with GOLD (r = -0.329, p = 0.001). Each Gln copy in the genotype correlated positively, and Glu copies negatively, with GOLD group D (Gln: r = 0.211, p = 0.035; Glu: r = -0.211, p = 0.035). Therefore, the Gln27Glu polymorphism could be involved in the pathogenesis of COPD and may be responsible for its severity.
When comparing groups with ANOVA analysis, there was no significant difference in age (р = 0.127), COPD duration (р = 0.136), and number of pack-years (р = 0.408). The Duncan’ multiple range test showed there was a tendency towards a difference in age between Gln27Gln and Glu27Glu groups (р = 0.051). Groups did not differ significantly by the number of exacerbations (р = 0.32), hospital admissions (р = 0.448), or out-patient exacerbations (р = 0.243) in the year prior to inclusions. There was also no difference in these parameters after 1 year of treatment (Table 3).
All study groups had improved significantly in terms of exacerbations (p < 0.001) and hospital admissions (p < 0.001 in Gln27Gln and Gln27Glu; p = 0.004 in Glu27Glu) in the year of tiotropium/olodaterol treatment. There was no significant improvement in the number of out-patient exacerbations for the Gln27Gln group (р = 0.168) or the Gln27Glu group (р = 0.442), however, a significant improvement was seen for the Glu27Glu group (р = 0.046).
There was no significant difference in the mMRC and CAT values at any visit between the study groups (Table 4). Using MANOVA method, there was a significant improvement in mMRC and CAT values in all groups over the course of the study (p < 0.001).
When comparing patients who required treatment with AB, there was a significant difference between the study groups (χ2 = 7.370; р = 0.025). There was no significant difference in patients who required GCS (χ2 = 3.353; р = 0.363) or xanthines (χ2 = 1.538; р = 0.463) (Table 5). There was a weak negative correlation between Gln copies (r = -0.258, p = 0.009), and a weak positive correlation between Glu copies (r = 0.258, p = 0.009), with antibiotic use. Additionally, Gln copies had a weak negative correlation (r = -0.275, p = 0.006), and Glu a weak positive correlation (r = 0.275, p = 0.006), with GCS use. In regression analysis, the Gln27Glu genotype increased risk of AB use by 12.4% [OR: 12.4%; 95% CI: 1.6%–23.33%; p = 0.025]. Therefore, the Gln27Glu genotype had an impact on utilization of different drug groups by the patients, with an increased risk of AB and GCS use for Gly copy carriers.
The average number of AB courses was 1.37 ± 0.16 in the Gln27Gln group, 1.59 ± 0.14 in the Gln27Glu group, and 2.00 ± 0.22 in the Glu27Glu group; this difference was close to the significance threshold (р = 0.052). There was no significant difference in the duration of AB treatment (p = 0.235). In correlation analysis, there was a weak negative correlation between Gln copies (r = 0.233, p = 0.02), and a weak positive correlation between Glu copies (r = 0.233, p = 0.02), and the number of AB courses. There was no significant difference in the number of GCS courses (р = 0.398) or xanthines courses (р = 0.407), as well as GCS (р = 0.341) and xanthines (р = 0.413) treatment duration (Table 6).
There was no significant improvement for patients requiring AB in all study groups after treatment with tiotropium/olodaterol. There was also no significant improvement for patients requiring GCS in the Gln27Gln group (χ2 = 2.331; р = 0.127). However, these improved for both the Gln27Glu group (χ2 = 4.387; р = 0.036) and the Glu27Glu group (χ2 = 12.396; р < 0.001). There was a significant difference between the study groups in the number of patients using GCS at the end of the study (χ2 = 7.585; р = 0.023). In correlation analysis, each Gln copy had a weak negative correlation (r = -0.275, p = 0.006), and Glu copies a weak positive correlation (r = 0.275, p = 0.006), with GCS use. In the regression model, each Glu copy increased the chances of GCS use by 15%. All study groups had improved in terms of xanthines use during the study (Table 7).
There was a significant difference in the number of antibiotics courses (p = 0.034), but not AB treatment duration (р = 0.124). In regression analysis each Glu copy prolonged AB treatment by 1.4 days [OR: 1.4; 95% CI: -0.1–2.95; p = 0.07], at the level of a tendency. There was also a significant difference in the number of GCS courses (p = 0.019) and GCS treatment duration (р = 0.014). There was a weak negative correlation between Gln copies with the number of GCS courses (r = -0.283, p = 0.004) and GCS treatment duration (r = -0.293, p = 0.003); and a weak positive correlation for Glu copies and GCS treatment duration (r = 0.241, p = 0.016). There were only tendencies found in the regression analysis. Therefore, each Glu copy increased the amount of GCS courses by 1.835 [OR: 1.835; 95% CI: -0.33–4,0; p = 0.096] and GCS treatment duration by 1.2 days [OR: 1.2; 95% CI: 0.0–2.45; p = 0.055]. There was no significant difference between the groups for the number of xanthines courses (p = 0.346) and treatment duration (p = 0.25) (Table 8).
The Gln27Gln group had significantly improved during the study for the number of AB courses (р = 0.001) and treatment duration, GCS courses (р = 0.002) and treatment duration (р = 0.001), and xanthines courses (р = 0.015) and treatment duration (р = 0.011). Gln27Glu group had significantly improved AB course number (р = 0.001) and treatment duration (p < 0.001) and GCS courses (р = 0.018) and treatment duration (р = 0.007). There was no improvement in the number of xanthines courses (р = 0.198) and treatment duration (р = 0.07). The Glu27Glu group showed improvement only in the use of antibiotics, with significant difference in the number of AB courses (р = 0.006) and treatment duration (p = 0.002). There was no improvement in the number of GCS courses (р = 0.782) and treatment duration (р = 0.791), as well as xanthines courses (р = 0.782) and treatment duration (р = 0.639).
Discussion
To date, there are five known single nucleotide polymorphisms of the ADRB2 gene, in positions 16, 19, 27, 34, 164 [18]. Yin et al. proved that polymorphisms in positions 16 (rs1042713, Arg→Gly) and 27 (rs1042714, Gln→Glu) decreased the function of ADRB218. Green et al. and Moore et al. showed a decrease in ADRB2 expression for the 16Arg/Gly polymorphism19, 20. These studies indicate an important role for genetic polymorphisms in the clinical course of COPD.
According to Katsarou et al., prevalence of Gln27Glu alleles in the European population is as follows: Gln27Gln — 42.80%, Gln27Glu — 45.84%, Glu27Glu — 11.36%21. In our study population, 35% had Gln27Gln, 39% had Gln27Glu, and 26% Glu27Glu. The higher prevalence of Glu27Glu alleles in COPD patients in our study might indicate a higher risk of COPD development in these patients, however, a study with more samples is required to prove this as the existing data is conflicting. Many studies state that the prevalence of the Gln27Glu polymorphism is higher in COPD patients, as is the risk of COPD development22, 23, 24, 25, while other alleles did not show this association26, 27, 28, 29.
In multiple studies, the Gln27Glu polymorphism did not affect the response to beta-2 agonists17, 30, 31. In our study, treatment with the tiotropium/olodaterol was effective at reducing the number of exacerbations and hospital admissions in all patients, independent of the ADRB2 gene polymorphism, however, we found differences in drug utilization between the study groups. We have not identified any studies that focused on the utilization of antibiotics and GCS in patients with COPD and specific ADRB2 gene polymorphisms.
In our study, we identified that the ADRB2 gene can be involved in protection against infection via an unknown mechanism, with Gln showing protective properties. Also, ADRB2 could be involved in crosstalk with other receptors at the cellular level, leading to altered communication between them. This could have caused the higher use of GCS in patients with Glu copies. The Gln27Gln genotype displayed a protective effect against both infections and GCS use.
Data obtained in the Rotterdam study indicated that Gln27 increased the risk of exacerbations in patients with COPD32. Similar data was presented by Ingebrigsten et al. who stated a higher risk of severe exacerbations in patients with Gln27Gln and Gln27Glu alleles, compared to the Glu27Glu allele33. In our study we failed to prove any relation between exacerbations and ADRB2 genes, contradicting the existing data. Overall, study results are conflicting and larger scale studies are required to determine the relation between ADBR2 gene polymorphisms and the clinical course of COPD, as well as investigations into the function of ADRB2 at the cellular level.
Conclusions
The ADRB2 gene is involved in the clinical progression of COPD and can increase its severity. Gln copies correlated negatively with GOLD group D for COPD, while Glu copies correlated positively, indicating different clinical severities between the study groups. However, no difference was seen for exacerbations. We showed that study groups utilized drugs differently, with each Gln copy associated with a smaller need for AB, as well as reduced number of courses and shorter treatment duration. Also, Gln copies were associated with reduced use of GCS after the 12 months of treatment with the LABA/LAMA combination. Treatment with the LABA/LAMA combination demonstrated a significant improvement of the COPD course in all study groups.
Abbreviations
AB: antibiotics, ADRB2: adrenoreceptor beta 2, CAT: COPD assessment tool, COPD: chronic obstructive pulmonary disease, GCS: glucocorticoids, mMRC: modified Medical Research Council
Acknowledgments
None.
Author’s contributions
Kostiantyn Dmytriiev: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Yuriy Mostovoy: Substantial contributions to the conception or design of the work; Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nataliis Slepchenko: the acquisition, analysis, or interpretation of data for the work; Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Dmytro Dmytriiev: Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Oleksandr Nazarchuk: Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Yuliia Smereka: Drafting the work or revising it critically for important intellectual content; Final approval of the version to be published; Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was conducted in accordance with the amended Declaration of Helsinki. The institutional review board approved the study, and all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
(GOLD)
Global Initiative for Chronic Obstructive Lung Disease,
Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (Online). https://www.goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf.
.
-
BOLD
Burden of Obstructive Lung Disease Initiative Webpage, published by Imperial College London. https://www.boldstudy.org/.
.
-
Lamprecht
B.,
McBurnie
M.A.,
Vollmer
W.M.,
Gudmundsson
G.,
Welte
T.,
Nizankowska-Mogilnicka
E.,
Collaborative Research Group
BOLD,
COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest.
2011;
139
(4)
:
752-63
.
View Article PubMed Google Scholar -
Blanco
I.,
Diego
I.,
Bueno
P.,
Casas-Maldonado
F.,
Miravitlles
M.,
Geographic distribution of COPD prevalence in the world displayed by Geographic Information System maps. The European Respiratory Journal.
2019;
54
(1)
:
1900610
.
View Article PubMed Google Scholar -
Mortality
GBD 2013,
Causes of Death Collaborators
Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet.
2015;
385
(9963)
:
117-71
.
View Article PubMed Google Scholar -
Lopez
A.D.,
Shibuya
K.,
Rao
C.,
Mathers
C.D.,
Hansell
A.L.,
Held
L.S.,
Chronic obstructive pulmonary disease: current burden and future projections. The European Respiratory Journal.
2006;
27
(2)
:
397-412
.
View Article PubMed Google Scholar -
Gaddam
S.,
Gunukula
S.K.,
Lohr
J.W.,
Arora
P.,
Prevalence of chronic kidney disease in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. BMC Pulmonary Medicine.
2016;
16
(1)
:
158
.
View Article PubMed Google Scholar -
Janson
C.,
Johansson
G.,
Ställberg
B.,
Lisspers
K.,
Olsson
P.,
Keininger
D.L.,
Identifying the associated risks of pneumonia in COPD patients: ARCTIC an observational study. Respiratory Research.
2018;
19
(1)
:
172
.
View Article PubMed Google Scholar -
Morgan
A.D.,
Zakeri
R.,
Quint
J.K.,
Defining the relationship between COPD and CVD: what are the implications for clinical practice?. Therapeutic Advances in Respiratory Disease.
2018;
12
:
1753465817750524
.
View Article PubMed Google Scholar -
Rasmussen
S.M.,
Brok
J.,
Backer
V.,
Thomsen
S.F.,
Meteran
H.,
Association Between Chronic Obstructive Pulmonary Disease and Type 2 Diabetes: A Systematic Review and Meta-Analysis. COPD.
2018;
15
(5)
:
526-35
.
View Article PubMed Google Scholar -
Silverman
E.K.,
Genetics of COPD. Annual Review of Physiology.
2020;
82
(1)
:
413-31
.
View Article PubMed Google Scholar -
Vacca
G.,
Schwabe
K.,
Dück
R.,
Hlawa
H.P.,
Westphal
A.,
Pabst
S.,
Polymorphisms of the beta2 adrenoreceptor gene in chronic obstructive pulmonary disease. Therapeutic Advances in Respiratory Disease.
2009;
3
(1)
:
3-10
.
View Article PubMed Google Scholar -
Karimi
L.,
Lahousse
L.,
Ghanbari
M.,
Terzikhan
N.,
Uitterlinden
A.G.,
van der Lei
J.,
β2-Adrenergic Receptor (ADRB2) Gene Polymorphisms and Risk of COPD Exacerbations: the Rotterdam Study. Journal of Clinical Medicine.
2019;
8
(11)
:
1835
.
View Article PubMed Google Scholar -
Stupnytska
G.,
Gorovenko
N.,
Podolska
S.,
Association of the ADRB2 gene polymorphic variant C79G (rs1072714) with the course of chronic obstructive pulmonary disease in obese and non-obese patients.. CBU International Conference Proceedings.
2018;
:
960-965
.
View Article Google Scholar -
Gorovenko
N.G.,
Stupnytska
G.Y.,
Podolskaya
S.V.,
Polymorphic variants of ADRB2, NR3C1, MDR1 genes as possible predictors of efficacy of combined therapy laba + ICS in patients with chronic obstructive pulmonary disease. The Pharma Innovation.
2014;
3
(8)
:
10-4
.
-
Hizawa
N.,
Makita
H.,
Nasuhara
Y.,
Betsuyaku
T.,
Itoh
Y.,
Nagai
K.,
Beta2-adrenergic receptor genetic polymorphisms and short-term bronchodilator responses in patients with COPD. Chest.
2007;
132
(5)
:
1485-92
.
View Article PubMed Google Scholar -
Kim
W.J.,
Oh
Y.M.,
Sung
J.,
Kim
T.H.,
Huh
J.W.,
Jung
H.,
Lung function response to 12-week treatment with combined inhalation of long-acting beta2 agonist and glucocorticoid according to ADRB2 polymorphism in patients with chronic obstructive pulmonary disease. Lung.
2008;
186
(6)
:
381-6
.
View Article PubMed Google Scholar -
Reihsaus
E.,
Innis
M.,
MacIntyre
N.,
Liggett
S.B.,
Mutations in the gene encoding for the beta 2-adrenergic receptor in normal and asthmatic subjects. American Journal of Respiratory Cell and Molecular Biology.
1993;
8
(3)
:
334-9
.
View Article PubMed Google Scholar -
Yin
K.,
Zhang
X.,
Qiu
Y.,
Association between beta2-adrenergic receptor genetic polymorphisms and nocturnal asthmatic patients of Chinese Han nationality. Respiration.
2006;
73
(4)
:
464-7
.
View Article PubMed Google Scholar -
Green
S.A.,
Turki
J.,
Innis
M.,
Liggett
S.B.,
Amino-terminal polymorphisms of the human beta 2-adrenergic receptor impart distinct agonist-promoted regulatory properties. Biochemistry.
1994;
33
(32)
:
9414-9
.
View Article PubMed Google Scholar -
Moore
P.E.,
Laporte
J.D.,
Abraham
J.H.,
Schwartzman
I.N.,
Yandava
C.N.,
Silverman
E.S.,
Polymorphism of the beta(2)-adrenergic receptor gene and desensitization in human airway smooth muscle. American Journal of Respiratory and Critical Care Medicine.
2000;
162
(6)
:
2117-24
.
View Article PubMed Google Scholar -
Katsarou
M.S.,
Karathanasopoulou
A.,
Andrianopoulou
A.,
Beta 1, Beta 2 and Beta 3 Adrenergic Receptor Gene Polymorphisms in a Southeastern European Population. Front Genet.
2018;
9
:
560
.
View Article PubMed Google Scholar -
Hegab
A.E.,
Sakamoto
T.,
Saitoh
W.,
Massoud
H.H.,
Massoud
H.M.,
Hassanein
K.M.,
Polymorphisms of IL4, IL13, and ADRB2 genes in COPD. Chest.
2004;
126
(6)
:
1832-9
.
View Article PubMed Google Scholar -
Hussein
M.H.,
Sobhy
K.E.,
Sabry
I.M.,
El Serafi
A.T.,
Toraih
E.A.,
Beta2-adrenergic receptor gene haplotypes and bronchodilator response in Egyptian patients with chronic obstructive pulmonary disease. Advances in Medical Sciences.
2017;
62
(1)
:
193-201
.
View Article PubMed Google Scholar -
Ganbold
C.,
Jamyansuren
J.,
Puntsag
O.,
ADRB2 and ACE gene polymorphisms in COPD susceptibility. Cent Asian J Med Sci..
2016;
2
(2)
:
127-33
.
-
Br∅gger
J.,
Steen
V.M.,
Eiken
H.G.,
Gulsvik
A.,
Bakke
P.,
Genetic association between COPD and polymorphisms in TNF, ADRB2 and EPHX1. The European Respiratory Journal.
2006;
27
(4)
:
682-8
.
View Article PubMed Google Scholar -
Papatheodorou
A.,
Makrythanasis
P.,
Kaliakatsos
M.,
Dimakou
A.,
Orfanidou
D.,
Roussos
C.,
Development of novel microarray methodology for the study of mutations in the SERPINA1 and ADRB2 genes\textemdashtheir association with Obstructive Pulmonary Disease and Disseminated Bronchiectasis in Greek patients. Clinical Biochemistry.
2010;
43
(1-2)
:
43-50
.
View Article PubMed Google Scholar -
Thomsen
M.,
Nordestgaard
B.G.,
Sethi
A.A.,
Tybj\aerg-Hansen
A.,
Dahl
M.,
β2-adrenergic receptor polymorphisms, asthma and COPD: two large population-based studies. The European Respiratory Journal.
2012;
39
(3)
:
558-66
.
View Article PubMed Google Scholar -
Vacca
G.,
Schwabe
K.,
Dück
R.,
Hlawa
H.P.,
Westphal
A.,
Pabst
S.,
Polymorphisms of the beta2 adrenoreceptor gene in chronic obstructive pulmonary disease. Therapeutic Advances in Respiratory Disease.
2009;
3
(1)
:
3-10
.
View Article PubMed Google Scholar -
Hizawa
N.,
Makita
H.,
Nasuhara
Y.,
Betsuyaku
T.,
Itoh
Y.,
Nagai
K.,
Beta2-adrenergic receptor genetic polymorphisms and short-term bronchodilator responses in patients with COPD. Chest.
2007;
132
(5)
:
1485-92
.
View Article PubMed Google Scholar -
Yelensky
R.,
Li
Y.,
Lewitzky
S.,
Leroy
E.,
Hurwitz
C.,
Rodman
D.,
A pharmacogenetic study of ADRB2 polymorphisms and indacaterol response in COPD patients. The Pharmacogenomics Journal.
2012;
12
(6)
:
484-8
.
View Article PubMed Google Scholar -
Karimi
L.,
Lahousse
L.,
Ghanbari
M.,
Terzikhan
N.,
Uitterlinden
A.G.,
van der Lei
J.,
β2-Adrenergic Receptor (ADRB2) Gene Polymorphisms and Risk of COPD Exacerbations: the Rotterdam Study. Journal of Clinical Medicine.
2019;
8
(11)
:
1835
.
View Article PubMed Google Scholar -
Ingebrigtsen
T.S.,
Vestbo
J.,
Rode
L.,
Marott
J.L.,
Lange
P.,
Nordestgaard
B.G.,
β2-Adrenergic genotypes and risk of severe exacerbations in COPD: a prospective cohort study. Thorax.
2019;
74
(10)
:
934-40
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 9 No 5 (2022)
Page No.: 5043-5050
Published on: 2022-05-31
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 4339 times
- PDF downloaded - 1462 times
- XML downloaded - 0 times
 Biomedpress
Biomedpress

