Cytokine-induced killer cell transplantation: an innovative adoptive therapy
Abstract
Cytokine-induced killer (CIK) cells areeffector immune cells with anti-tumor potency of T lymphocytes as well as non-major histocompatibility complex restricted elimination of natural killer cells. Preclinical models have shown that CIK cells have strong anti-tumor killing capacity against a variety of blood cancers and solid tumors. Clinical studies confirm the advantages of CIK cells, including the safety of CIK cell therapy in patients with advanced cancer. A preeminent property of CIK cells, which may help them to overcome some of the limitations of other adoptive immunotherapy strategies, is their ability to be expanded ex vivo to high numbers. Their robust in vitro proliferation provides adequate quantity for multiple adoptive infusions. The tumor-killing capacity of CIK cells is mainly based on the interaction between NKG2D molecules on CIK cells and MIC A/B or ULBP molecules on tumor cells. Moreover, CIK cells have a reduced allo-reactivity across HLA-barriers. This review summarizes the clinical applications of CIK cells and updates of combining CIK cells with other therapies. This review highlights the benefits of CIK cell use in clinical treatment of cancer.
Introduction
In spite of the burst in the development and application of new targeted approaches for cancer, still many cancers remain poorly treatable. In recent trends of adoptive cellular therapy, the application of cytokineinduced killer (CIK) cells has been seen as an innovative strategy with encouraging anti-cancer potency. CIK cells activated in vitro can co-possess properties of T cells and NK cells, displaying both potent antitumor ability of T lymphocytes and also non-major histocompatibility complex (MHC) restricted tumor cell killing of natural killer (NK) cells Laport et al., 2011. CIK cells are a heterogeneous cell population that include CD3+CD56+ cells, CD3-CD56+ NK cells and CD3+CD56- T cells. Preclinical studies in mouse models have indicated that CIK cells have strong antitumor immunity against blood cancers and solid tumors. Clinical studies further confirm the benefit and safety of CIK cell therapy in patients with malignant disease Jiang et al., 2013.
CIK cells have the potential to overcome the main barriers which have hindered the “bench to bedside” applications of adoptive immunotherapy. Part of their appeal is the ease by which they can be isolated, the low-cost of expansion and their robust proliferation from mononuclear blood cells. Since CIK cells can be grown to high cell numbers, this allows for multiple adoptive infusions Sangiolo, 2011. NKG2D molecules expressed on CIK cells play an important role in the effector-target interaction by binding to MIC A/B or ULBPs molecules expressed on tumor cells. Finally, since CIK cell recognition of cancer cells occurs in a non-HLA restricted fashion, CIK cells can be used widely for clinical applications involving allogeneic cell transplant Sangiolo, 2011. It is not surprising, given the advantages mentioned above, that CIK cells have been currently implemented in numerous clinical trials for a number of neoplastic diseases Guo and Han,2015. This review summarizes the advantages of CIK cells among other immunotherapies and provides updates of recent CIK cell trials for cancer, particularly in combination with other therapies.
CIK cell treatment of varied types of cancer
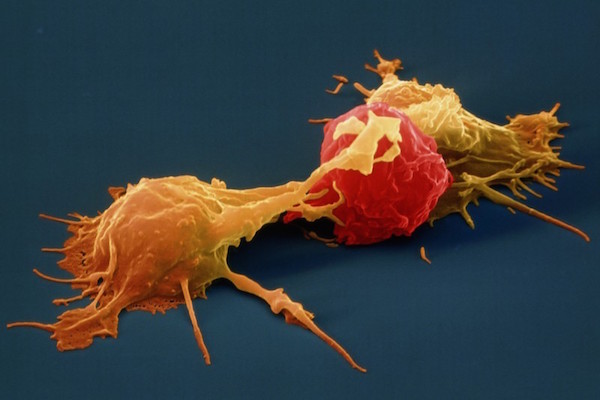
The CD3+CD56+ -expressing cell population of CIK cells is responsible for the anti-tumor cytolytic activity. The main mechanism of CIK activation is via ligation of the surface activating receptors, e.g. NK group 2, member D (NKG2D), DNAX accessory molecule 1 (DNAM-1) and lymphocyte function-associated antigen 1 (LFA-1). LFA-1 interacts with its ligand on tumor cells to link effector-target binding; signals through NKG2D and DNAM-1 lead to full CIK cell activation. Upon stimulation, CIK cells induce granule exocytosis, cytokine secretion and cancer cell cytotoxicity Pievani et al., 2011.
CIK cell therapy in the treatment of hematological malignancies
CIK cells generated from bone marrow of acute myeloid leukemia (AML) samples not only show cytotoxicity against autologous AML targets but also allogeneic cognate malignant cells. In mouse models, although donor splenocytes induced a strong graft vs. host disease (GvHD), CIK cells did not. As a result, the infusion of CIK cells helped to prolong survival time of murine leukemia-bearing mice. Interestingly, the Linn et al. realized that CIK cells could interact with dendritic cells (DC) to enhance the cytolytic activity against target cells Linn and Hui, 2003. Laport et al. explored the cytotoxic capability of CIK cells and showed that CIK cell-mediated adoptive immunotherapy is safe and induces only a low incidence of GvHD. Thus, the use of CK cells in adoptive immunotherapy is a promising way to enhance graft-versustumor responses Laport et al., 2011.
Introna et al. showed they can produce CIK cells from very low quantity of nucleated cells isolated from cord blood. CIK cells in the study showed direct cytotoxicity against several tumor cell lines, including B lymphomas, T lymphomas and myeloid leukemias. In accordance with other research studies, CIK cells were shown to highly express cytolytic granules, such as perforin, granzyme and NKG2D molecule. Nowadays, CIK cells are easily generated under GMP standards; therefore, it is possible that in the near future there may be increased clinical applications of CIK cells in leukemia following cord blood transplantation Introna et al.,2006.
Co-incubation CIK cells and chronic lymphocytic leukemia (CLL) cells accelerated ICAM-1 expression and apoptosis ratio of CLL targets. These effects were mainly reliant on CIK cell-mediated secretion of IFNgamma (IFN-g) secretion, an important cytokine in modulating expression of adhesion molecules on CLL cells Kornacker et al., 2006a. Clinically, CIK cells were applied to treat autologous advanced recurrent acute myeloid leukemia (AML) patients. Expectedly, the leukemic cell signal dropped to almost undetectable level. Analysis of AML-derived CIK cells showed that they were capable of secreting high levels of type I immune-promoting cytokines (interleukin-2 (IL-2), IFN-g and tumor necrosis factor-alpha (TNF-a)) Wang et al.,2013b. In the trend of clinical studies, CIK cells demonstrated an important influence on the treatment of hematological malignancies, which are based on some critical parameters, including remissions, survival durations and quality of life. Further research needs to be done to elucidate the parameters for optimal application schedule of CIK in clinical practice Schmeel et al., 2014.
CIK against lung adenocarcinoma
CIK cells were able to improve the immune function of lung cancer patients Jin et al., 2013. It is wellknown that the first signal for CIK cell activation is based on the interaction between MHC class I chainrelated gene A (MICA) expressed on the tumor cell and its related ligand on the effector cell. Chen et al. explored the clinical significance of MICA expression in patients with advanced non-small cell lung cancer (NSCLC) and the efficacy of CIK therapy. The authors found that MICA expression correlated with the stage of lung cancer. Moreover, patients who were treated with CIK cell therapy and who had high MICA expression showed enhanced overall survival compared to those with low expression Chen et al., 2013. Wang et al. systemically evaluated randomized controlled trials of CIK cells for the treatment of NSCLC. In that analysis, CIK cell therapy significantly improved the objective response rate and overall survival. Interestingly, the authors concluded that CIK cell adoptive therapy combined with other therapies should have great superiority in enhancing patient survival as well as anti-tumor immunity. Moreover, the innovative CIK cell therapy did not present any evidence of major adverse events in the NSCLC patients Wang et al., 2014a.
The standard protocol for culturing CIK cells entails growing mononuclear cells (MNC) in a timedependent manner with 3 kinds of stimulants, including IFN-g, anti-CD3 monoclonal antibody and IL-2 (widely used cytokine which is refreshed all throughout the culture period). Although the role of IL-2 is in maintaining the proliferative signal in effector cells, its use in the clinical setting is controversial Wang et al., 2014b. For that reason, many researchers have replaced or combined IL-2 with IL-15. For instance, Wei et al. stimulated the CIK cells by combining IL-2 and IL-15 to achieve enhanced cytotoxicity against lung cancer cells since IL-15 offers an alternative stimulant for the expansion of CD3+CD56+ subset and enhanced cytotoxicity against tumor cells. In a tumor-bearing mouse model, the transfusion of CIK cells cultured in IL-2 & IL-15 conditioned medium showed significant tumor regression Wei et al., 2014.
CIK applications for the treatment of gastrointestinal malignant diseases
After activation, CIK cells induce target cell apoptosis which can be easily observed through the appearance of cell-death markers, such as condensed chromatin, disintegration of the nucleolus, vacuoles in the cytoplasm and “apoptotic bodies”. Sun et al. demonstrated the apoptotic events which occurred in a gastric cancer cell line following interaction with CIK cells, via scanning electron microscope and transmission electron microscopy Sun et al., 2005. Gene expression analysis also showed that C-myc and Bcl-2 were significantly down-regulated, and that expression of Bax was increasingly up-regulated as time of co-culture increased Sun et al., 2005.
During the differentiation process, the quantity of CIK cells reaches the maximal peak between days 14 to 21; the maximal cytotoxic activity is also reached at this time. Therefore, CIK cells should be collected between the 14 to 21 days culture period for the highest quantity and quality. During this time, there is a harmonious balance between differentiation status, cytotoxic activity and survival time, which are optimal factors for clinical applications of CIK cells. Given the advantages of CIK cells, researchers have begun to evaluate CIK as an innovative addition to conventional therapies to reduce the adverse effects of standard therapies. Jiang et al. investigated the effects of chemotherapy plus CIK cells in advanced gastric cancers patients Jiang et al., 2006. The results showed that tumor markers in peripheral blood were significantly decreased. Additionally, there were other encouraging results, including improved host immune function, augmented curative effect, increased survival time, and improved quality of life in CIK + chemotherapy treated patients, compared to those treated with chemotherapy alone Jiang et al., 2006. The more frequent the CIK cell transfusion, the lower the risk of death in gastric cancer patients Jiang et al., 2010.
One of the worst side effects of traditional therapies for cancer is that they do not specifically target cancer cells. Repeated schedule treatments often increase the risk of creating a new malignant subpopulation with therapy-resistant characteristics. Oxaliplatin (L-OHP) is a platinum-based antineoplastic agent used in cancer chemotherapy. Inappropriate treatment of gastric cancer with oxaliplatin can produce oxaliplatinresistant cancer cells; however, the combination of oxaliplatin and CIK cells was shown to reverse chemoresistance Zhao et al., 2010. In vitro studies have shown that combination of CIK cells and L-OHP could significantly enhance anti-tumor killing activity, even of oxaliplatin-resistant cells. Moreover, in vivo results have also demonstrated enhanced synergetic effects against oxaliplatin-resistant cells when the two therapies were combined Zhao et al., 2010. In another study S-1 (Tegafur, Gimeracil, and Oteracil Potassium Capsules) plus CIK were evaluated in patients with advanced pancreatic cancer. In these patients, serum CA19-9 levels significantly decreased and the time to progression was longer. Clinically, the side effects frequently associated with chemotherapy, including nonhematological toxicity, fatigue and non-infective, were significantly decreased in the combined therapy groups Wang et al., 2013a.
One of the main issues, particularly for cell-based immunotherapies in cancer treatment, which needs to be satisfactorily resolved is the issue of safety. And how can effector cells that are transfused into the patient's body by cell-based immunotherapy be rendered more efficient than traditional therapies? How can they augment traditional therapies? Jakel et al. summarized recent clinical studies which applied CIK cells for the treatment of gastric, pancreatic, hepatocellular and colorectal cancer. Cytotoxic cells were grafted by various routes, including intravenously, intraperitoneally, or via the common hepatic artery. In all the studies, the side effects and toxicity of CIK cell therapy were mild. In cancer patients, malignant cells can create a micro-environment with components preventing the effector cell penetration. However, CIK cells represent an effective way to activate the immune system to overcome the barriers and destroy cancer cells. Not surprisingly, the combinational therapy (of CIK cell therapy with conventional adjuvants) can be highly effective over a single therapy, as demonstrated in GI cancer Jakel et al., 2014.
CIK therapy in treating patients with liver cancer
Before CIK cells, other kinds of effector cells were used in adoptive cellular therapy (ACT), namely lymphokine- activated killer (LAK) cells and tumorinfiltrating lymphocytes (TIL). The main common features of TIL and LAK cells are that they can specifically recognize the cancer cell targets and induce cell killing. However, the biggest obstacle to their clinical use is their limited in vitro proliferation. CIK cells, however, maintain their robust proliferation during in vitro culture and have potent anti-tumor cytotoxicity.
Liver cancer is one of the most fatal cancers, and is strongly associated with chronic infection of HBV or HCV. Among primary liver cancers, hepatocellular carcinoma (HCC) represents the major histologic type. Wan, et al. used autologous CIK cells to develop an alternative adoptive therapeutic strategy for HCC patients. The author cultured CIK cells from healthy donors and HCC patients and found that after 21 days of incubation, CD3/CD56 double-positive cells significantly increased. The in vitro and in vivo assays affirmed CIK cells originating from HCC patients eliminated autologous tumor cells much better than autologous LAK cells and PBMC cells Wang et al., 2002.
Zhang et al. investigated CIK treatment of postoperated HCC patients who expressed multidrugresistant (MDR) proteins. The authors found a high number of activated lymphocytes infiltrated in the liver cancer tissue via immunohistochemistry. CIK cells effectively lysed MDR HCC cells; moreover, CIK cells were a safe adoptive immunotherapy without side effects Zhang et al., 2005. Ma et al. compared the outcome of HCC treatment with or without CIK cell intervention. The group receiving CIK had significantly favored outcomes and the treatment also diminished HBV-DNA content and AFP level Ma et al., 2012.
Combination CIK and other targeted therapy
CIK cell adoptive transfer is increasingly playing an important role in cancer treatment. Combining CIK cells with other established therapies represents a highly promising approach among immunotherapy strategies for cancer treatment.
CIK cell with dendritic cell (DC)
While CIK cells may forcefully destroy cancer cells in vitro; in vivo results may not reflect the potential impact of CIK cells. Part of the reason is that once CIK cells are injected into the body, they need the support other immune cells, e.g. antigen-presenting cells. Dendritic cells (DC) are professional antigenpresenting cells with the ability to synergize the immune system and induce appropriate regulatory mechanisms. For these reasons, DC have garnered interest from many researchers. Of further interest is the combination of CIK and DC in cancer therapy. The relationship between DC and CIK cells is not a oneway interaction but one that is reciprocal For instance, when CIK cells are activated by DC, they secrete factors which further enhance the activating status of DC Li et al., 2009.
After co-culture with CIK cells, DC show upregulation of co-stimulatory and antigen-presenting molecules, as well as IL-12 secretion; this feedback leads to enhanced cytotoxic activity of CIK cells against the malignant cells Marten et al., 2001. Studies have reported from DC-CIK cell co-culture distinct changes in expression of surface molecule markers on both cell populations Nagaraj et al., 2004. Wongkajornsilp et al. pre-incubated CIK cells with tumor's RNA-primed DCs and showed an enhanced cytolysis of the osteosarcoma Wongkajornsilp et al., 2005. The existence of many immune components in a tight microenvironment is one of many reasons why the immune system may fail to adequately destroy tumor cells. For effective osteosarcoma cytolysis, CIK cells had to be kept at limited cell density with the help of tumor antigen presentation on DC Wongkajornsilp et al., 2005.
When Wei et al. compared cord blood DC-CIK cells, cord blood CIK cells and peripheral blood DC-CIK cells, he found that the proliferation capability of cord blood DC-CIK cells was the highest Wei et al., 2008, as was their activity against all subtypes of acute leukemia cells Wei et al., 2010. This suggests the possibility of using cord blood-derived MNC cells to differentiate DC and CIK cells for treatment application, opening up the prospect of treatment for patients with leukemia after hematopoietic stem cell transplant. One issue of concern for the acquisition of immune cells from cancer patients is that the low number of cells that can be obtained. Typically, from patient samples there are not sufficient enough precursor cells to expand to high enough numbers during ex vivo stimulation. The low numbers of acquired immune cells are likely are result of advanced disease stage and repeated chemotherapy or radiation therapy. Some patients deny acquisition of their immune cells based on a fear that blood collection may not be safe.
In their studies, Wang et al. showed that semiallogeneic DC-CIK cells were superior to autologous CIK cells and DC-CIK cells in terms of anti-tumor activity, IFN-g secretion, ratio of CD3+CD56+ cells, and promotion of cell proliferation. Furthermore, semiallogeneic DC-CIK cells reduced IL-4/IL-10 secretion, decreased the number of CD4+CD25+ cells, and lessened cell apoptosis Schmidt et al., 2004Wang et al., 2010. In clinical trials, Yang, et al. performed a paired study between chemotherapy plus DC + CIK cells versus control (chemotherapy alone) in patients with advanced NSCLC. DC-activated CIK cells significantly enhanced antitumor activity, increased the ratio of CD3+CD56+ cells, promoted cell proliferation, lessened cell apoptosis, and increased overall survival rates Yang et al., 2013. These data are in harmony with results from other studies, which showed that DC-CIK therapy increased the survival rates and progression free survival, compared to placebo, no intervention, conventional treatments, or other complementary and alternative medicines Chen et al., 2014. Yuanying et al. also showed that combining cryosurgery, chemotherapy or DC therapy with activated CIK immunotherapy can help prolong the median overall survival of patients Yuanying et al., 2013.
For DC, the selection of antigens for inducing maturation play a role in educating effector cells to destroy cancer cells expressing that antigen. Tumor antigens may be derived from RNA or protein. The selection of suitable antigens depends on the cancer type. There is a method to help acquire the cancer type-independent tumor antigens (protein antigens) from tumor lysis. Wang et al. used CIK cells co-cultured with DCs pulsed with complete retinoblastoma antigens (DCAg). CIK cells showed enhanced differentiation and cytotoxicity even on carboplatin-resistant RB cells; DC-Ag-CIK mixture had little effect on normal retina Wang et al., 2013c.
In the case of cancer patients forced to transplant immune cells more than once, patients can have adverse side effects if using effector cells like LAK for infusion. However, CIK cell transfusion has no harmful side effects. Zhao et al. withdraw peripheral blood mononuclear cells (PBMC) and expanded DC-CIK cells, then transfused multiple infusions in cancer patients. He found the cellular immunity was improved as the numbers of infused cytotoxic T lymphocytes (CTL) were increased Zhao et al., 2015.
CIK with specific antibodies
One of the most widely targeting strategies is cancer cell specific antibody carrying radioactive particles (used in radiotherapy) or drug precursors (used in chemotherapy). Today, the use of bi-specific antibodies (bsAb) have been studied in anti-cancer immunotherapy. The benefits of this strategy is that antibodies can be designed to have specific recognition sequences of antigens on cancer cells; the bi-specific antibody also provides binding sequences of effector cells. The specific recognition results in increased cohesion between cancer cells and immune cells, thereby inducing targeted and prolonged cell killing activity
Cancer cells have the ability to maintain growth in the patient's body without being diminished by the immune system, partly due to the fact that cancer cells originate from normal cells. Once mutation have accumulated enough, cancer cells form a microenvironment which protects them against the infiltration of immune cells. The difference between a malignant cell and normal cell can be abnormal expression, mainly overexpression, of growth factor receptor molecules on the cell surface, which have an important role in promoting cancer cell replication. Chan et al. collected cancer cells and autologous CIK cells from ovarian cancer patients. CIK cells with enhancement by bispecific antibodies against cancer antigen-125 and Her2 showed a significant increase in the mean percent lysis of ovarian cancer cells. The same result was duplicated in a mouse model; CIK cells with bispecific antibodies had significant reduction in tumor burden and improvement in survival Chan et al., 2006. In another study, both anti-tumor activity and CIK cell proliferation were increased when redirected to breast and ovarian cell tumor targets with bsAb Kornacker et al., 2006b.
In order to combine the benefits of antibody and CIK cells, researchers have designed CIK cells with a chimeric receptor specific for a desired antigen, i.e. chimeric antigen receptor (CAR). This can be done easily using molecular biology tools. CAR-CIK cells, which are activated by corresponding antigens, can be activated immediately without waiting for the second signal (classic TCR). This overcome obstacles in the tumor microenvironment where the second or third signal is difficult to express due to the presence of immunosuppressive factors. Although CAR gene transfer into CIK cells is possible, whether modified- CIK cells maintain the same properties as the parental cell needs to be evaluated. Marin et al. redirected CIK cells with CAR specific for CD19. The modified-CIK cells maintained the presentation of chemotactic molecules, such as CXCR4, CCR6 and CCR7. The modified CIK cells transmigrated through endothelial cells and showed B-ALL cell cytotoxicity Marin et al., 2006. In another study, Yoon et al. electroporated to CIK cell Her-2/neu-CAR. Compared with Herceptin (monoclonal antibody specific for Her-2/neu) CAR-CIK led to significant inhibition of Her-2/neu-positive tumor growth Yoon et al., 2009.
Tumors contain a small subpopulation with stem cell characteristics, called cancer stem cells (CSC). Stem cells are of tumor origin, maintain tumor growth, and show metastatic capability. Many cancer studies have focused on identifying the CSC characteristics. Huang et al. bound CD133-CAR to the CIK cells and found that these BsAb-CIK cells inhibited the survival of CD133 (high). CSCs eliminated pancreatic and hepatic cancer cells in vitro as well as in tumor-bearing nude mice Huang et al., 2013.
The international registry on CIK cells (IRCC)
Many studies on CIK cells have been published, including clinical trials involving large numbers of patients around the world with different cancer types. The studies were initiated based on the recognition of the certain advantages of CIK cells, particularly combined with standard cancer therapies, in eradicating disease. However, these studies are international and ideally require development of an organized registry to collect and evaluate data from all the clinical trials that have utilized CIK cells. From there, clinicians, researchers and patients will have meaningful data to compare and choose appropriate treatments Hontscha et al.,2011.
An international registry on CIK cells has recently been established. With statistics from clinical trials, the registry appears to set the systemic standard that publications must follow. The outcomes of the CIK cell treatment have been documented, which include increased overall survival rate, improved quality of life, minor adverse reactions, and importantly, enhanced immunologic effects, including accelerated cytotoxic T cell subsets and cytokine secretion, and decreased tumor markers and viral infection. There are now over 45 studies present in the database reported on 22 different tumor entities altogether enrolling around 3,000 patients. CIK cells have gained major strides as a promising immunotherapy platform in oncology Schmeel et al., 2015.
CIK in GvHD
After transplantation, donor cell rejection may occur, or sometimes GvHD, wherein the graft cells attack the recipient’s. The latter case is very hazardous since patients often experience immunosuppressive episodes before cell transplantation. This makes the patient susceptible to infectious agents since they are unable to activate appropriate immune responses. The attack of exogenous immune cells in an immuno-deficient body may cause impaired quality of life and even fatality for some patients. In cancer patients, optimal effector cell transplant involves achieving graft-versus-tumor responses with minimal GvHD. Reports have demonstrated that CIK cells show strong lytic activity against several tumor targets with acceptable GvHD, even when a large number of effector CIK cells are transplanted. The mechanism of reduction in GvHD is related to the ability of CIK cells to produce high levels of IFN- γ Baker et al., 2001. This results from the fact that IFN-γ, or type II interferon, play a crucial role in immune systems with the most potency of immunomodulation Schoenborn and Wilson, 2007Schroder et al., 2004. Besides, CIK cells have shown slow division rate and high susceptibility to apoptosis, while demonstrating low infiltration into GvHD target tissues Nishimura et al.,2008 and inducing low tissue damage Zhang et al., 2015.
CIK with regulatory T cells (Tregs)
The immune system is comprised of a coordinated network of cells, specialized to activate immune factors when the body is infected by infection or cancer, thereby destroying harmful agents to cells, tissues, organs and the whole body. When an immune reaction occurs effectively, the pathogen is eliminated. However, the body can also be damaged in the process; thus, immune regulation is also needed to minimize overactivation that can result in autoimmunity. CD4+CD25+ regulatory T (Treg) cells are professional regulatory cells which play an important role in maintaining a balanced immune system. The existence of Treg cells in cell culture suspension can be a mechanism of immune suppression, and result in the strong inhibition of anti-tumor effector cells.
In CIK cell culture, one of the most important components needed for the differentiation of CIKs is IL-2. Signaling pathway through IL-2 receptor plays an important role in maintaining the proliferative and cytotoxic properties of CIK cells. The IL-2 receptor is expressed by many different effector cells and activation can be induced by exogenous IL-2. MNC cultured with exogenous IL -2 could be induced to proliferate and differentiate into various effector cell populations, including Treg cells Koreth et al., 2011Matsuoka et al.,2013. Although CIK cells in culture suspension may increase in cell number, their cytotoxic activity has been shown to be significantly reduced, which may adversely affect the success of ACT Sakaguchi et al., 2009Sakaguchi et al., 2008. After Treg depletion at the start of CIK cell culture, however, the proliferation and cytotoxicity of cytotoxic cells are significantly increased, and CIK-mediated suppression of lung cancer cells both in vitro and in vivo are enhanced Li et al., 2007.
Conclusion
CIK adoptive immunotherapy has increasingly become a popular and effective new platform in cancer treatment, with numerous CIK clinical trials conducted worldwide to treat various cancers. Specifically, the ease of generating large amounts of CIK cells and their MHC-unrestricted tumor killing had led to their favorable use in cancer clinical translational studies. CIK have been successively studied in vitro and in vivoagainst a variety of cancers, and have consistently been shown to be effective killers. More investigations of CIK cells, particularly in the combination setting, i.e. synergized with conventional chemotherapy, targeted therapies and other immunotherapy approaches, are encouraged. Given their advantageous properties, it is evident that CIK cells will continue to show promise in anti-tumor adoptive immunotherapy.
References
-
J.
Baker,
M.R.
Verneris,
M.
Ito,
J.A.
Shizuru,
R.S.
Negrin.
Expansion of cytolytic CD8(+) natural killer T cells with limited capacity for graft-versus-host disease induction due to interferon gamma production. Blood.
2001;
97
:
2923-2931
.
-
J.K.
Chan,
C.A.
Hamilton,
M.K.
Cheung,
M.
Karimi,
J.
Baker,
J.M.
Gall,
S.
Schulz,
S.H.
Thorne,
N.N.
Teng,
C.H.
Contag.
Enhanced killing of primary ovarian cancer by retargeting autologous cytokine-induced killer cells with bispecific antibodies: a preclinical study. Clinical cancer research : an official journal of the American Association for Cancer Research.
2006;
12
:
1859-1867
.
-
R.
Chen,
X.
Deng,
H.
Wu,
P.
Peng,
B.
Wen,
F.
Li,
F.
Li.
Combined immunotherapy with dendritic cells and cytokineinduced killer cells for malignant tumors: a systematic review and metaanalysis. International immunopharmacology.
2014;
22
:
451-464
.
-
Y.
Chen,
G.
Lin,
Z.Q.
Guo,
Z.F.
Zhou,
Z.Y.
He,
Y.B.
Ye.
Effects of MICA expression on the prognosis of advanced nonsmall cell lung cancer and the efficacy of CIK therapy. PloS one.
2013;
8
:
e6904-4
.
-
Y.
Guo,
W.
Han.
Cytokine-induced killer (CIK) cells: from basic research to clinical translation. Chinese journal of cancer.
2015;
34
:
6
.
-
C.
Hontscha,
Y.
Borck,
H.
Zhou,
D.
Messmer,
I.G.
Schmidt-Wolf.
Clinical trials on CIK cells: first report of the international registry on CIK cells (IRCC). Journal of cancer research and clinical oncology.
2011;
137
:
305-310
.
-
J.
Huang,
C.
Li,
Y.
Wang,
H.
Lv,
Y.
Guo,
H.
Dai,
M.S.
Wicha,
A.E.
Chang,
Q.
Li.
Cytokine-induced killer (CIK) cells bound with anti-CD3/anti-CD133 bispecific antibodies target CD133(high) cancer stem cells in vitro and in vivo. Clinical immunology.
2013;
149
:
156-168
.
-
M.
Introna,
M.
Franceschetti,
A.
Ciocca,
G.
Borleri,
E.
Conti,
J.
Golay,
A.
Rambaldi.
Rapid and massive expansion of cord bloodderived cytokine-induced killer cells: an innovative proposal for the treatment of leukemia relapse after cord blood transplantation. Bone marrow transplantation.
2006;
38
:
621-627
.
-
C.E.
Jakel,
A.
Vogt,
M.A.
Gonzalez-Carmona,
I.G.
Schmidt-Wolf.
Clinical studies applying cytokine-induced killer cells for the treatment of gastrointestinal tumors. Journal of immunology research.
2014;
2014
:
89721-4
.
-
J.
Jiang,
C.
Wu,
B.
Lu.
Cytokine-induced killer cells promote antitumor immunity. Journal of translational medicine.
2013;
11
:
83
.
-
J.
Jiang,
N.
Xu,
C.
Wu,
H.
Deng,
M.
Lu,
M.
Li,
B.
Xu,
J.
Wu,
R.
Wang,
J.
Xu.
Treatment of advanced gastric cancer by chemotherapy combined with autologous cytokine-induced killer cells. Anticancer research.
2006;
26
:
2237-2242
.
-
J.T.
Jiang,
Y.P.
Shen,
C.P.
Wu,
Y.B.
Zhu,
W.X.
Wei,
L.J.
Chen,
X.
Zheng,
J.
Sun,
B.F.
Lu,
X.G.
Zhang.
Increasing the frequency of CIK cells adoptive immunotherapy may decrease risk of death in gastric cancer patients. World journal of gastroenterology : WJG.
2010;
16
:
6155-6162
.
-
C.G.
Jin,
X.Q.
Chen,
J.
Li,
Z.P.
Wu,
X.
Liu,
X.C.
Wang.
Moderating effects and maintenance of lung cancer cellular immune functions by CIK cell therapy. Asian Pacific journal of cancer prevention :.
2013;
APJCP14
:
3587-3592
.
-
J.
Koreth,
K.-i.
Matsuoka,
H.T.
Kim,
S.M.
McDonough,
B.
Bindra,
E.P.I.
Alyea,
P.
Armand,
C.
Cutler,
V.T.
Ho,
N.S.
Treister.
Interleukin-2 and Regulatory T Cells in Graft-versus-Host Disease. New England Journal of Medicine.
2011;
365
:
2055-2066
.
-
M.
Kornacker,
G.
Moldenhauer,
M.
Herbst,
E.
Weilguni,
F.
Tita-Nwa,
C.
Harter,
M.
Hensel,
A.D.
Ho.
Cytokine-induced killer cells against autologous CLL: direct cytotoxic effects and induction of immune accessory molecules by interferon-gamma. International journal of cancer Journal international du cancer.
2006a;
119
:
1377-1382
.
-
M.
Kornacker,
M.
Verneris,
B.
Kornacker,
T.
Ganten,
C.
Scheffold,
R.
Negrin.
The apoptotic and proliferative fate of cytokineinduced killer cells after redirection to tumor cells with bispecific Ab. Cytotherapy.
2006b;
8
:
13-23
.
-
G.G.
Laport,
K.
Sheehan,
J.
Baker,
R.
Armstrong,
R.M.
Wong,
R.
Lowsky,
L.J.
Johnston,
J.A.
Shizuru,
D.
Miklos,
S.
Arai.
Adoptive immunotherapy with cytokine-induced killer cells for patients with relapsed hematologic malignancies after allogeneic hematopoietic cell transplantation. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation.
2011;
17
:
1679-1687
.
-
H.
Li,
C.
Wang,
J.
Yu,
S.
Cao,
F.
Wei,
W.
Zhang,
Y.
Han,
X.B.
Ren.
Dendritic cell-activated cytokine-induced killer cells enhance the anti-tumor effect of chemotherapy on non-small cell lung cancer in patients after surgery. Cytotherapy.
2009;
11
:
1076-1083
.
-
H.
Li,
J.P.
Yu,
S.
Cao,
F.
Wei,
P.
Zhang,
X.M.
An,
Z.T.
Huang,
X.B.
Ren.
CD4 +CD25 + regulatory T cells decreased the antitumor activity of cytokine-induced killer (CIK) cells of lung cancer patients. Journal of clinical immunology.
2007;
27
:
317-326
.
-
Y.C.
Linn,
K.M.
Hui.
Cytokine-induced killer cells: NK-like T cells with cytotolytic specificity against leukemia. Leukemia & lymphoma.
2003;
44
:
1457-1462
.
-
Y.
Ma,
Y.C.
Xu,
L.
Tang,
Z.
Zhang,
J.
Wang,
H.X.
Wang.
Cytokine-induced killer (CIK) cell therapy for patients with hepatocellular carcinoma: efficacy and safety. Experimental hematology & oncology.
2012;
1
:
11
.
-
V.
Marin,
E.
Dander,
E.
Biagi,
M.
Introna,
G.
Fazio,
A.
Biondi,
G.
D'Amico.
Characterization of in vitro migratory properties of anti-CD19 chimeric receptor-redirected CIK cells for their potential use in B-ALL immunotherapy. Experimental hematology.
2006;
34
:
1219-1229
.
-
A.
Marten,
C.
Ziske,
B.
Schottker,
S.
Renoth,
S.
Weineck,
P.
Buttgereit,
F.
Schakowski,
A.
von Rucker,
T.
Sauerbruch,
I.G.
Schmidt- Wolf.
Interactions between dendritic cells and cytokineinduced killer cells lead to an activation of both populations. Journal of immunotherapy.
2001;
24
:
502-510
.
-
K.
Matsuoka,
J.
Koreth,
H.T.
Kim,
G.
Bascug,
S.
McDonough,
Y.
Kawano,
K.
Murase,
C.
Cutler,
V.T.
Ho,
E.P.
Alyea.
Low-dose interleukin-2 therapy restores regulatory T cell homeostasis in patients with chronic graft-versus-host disease. Science translational medicine.
2013;
5
:
179ra143
.
-
S.
Nagaraj,
C.
Ziske,
I.G.
Schmidt-Wolf.
Human cytokineinduced killer cells have enhanced in vitro cytolytic activity via non-viral interleukin-2 gene transfer. Genetic vaccines and therapy.
2004;
2
:
12
.
-
R.
Nishimura,
J.
Baker,
A.
Beilhack,
R.
Zeiser,
J.A.
Olson,
E.I.
Sega,
M.
Karimi,
R.S.
Negrin.
In vivo trafficking and survival of cytokine-induced killer cells resulting in minimal GVHD with retention of antitumor activity. Blood.
2008;
112
:
2563-2574
.
-
A.
Pievani,
G.
Borleri,
D.
Pende,
L.
Moretta,
A.
Rambaldi,
J.
Golay,
M.
Introna.
Dual-functional capability of CD3+CD56+CIK cells, a T-cell subset that acquires NK function and retains TCRmediated specific cytotoxicity. Blood.
2011;
118
:
3301-3310
.
-
S.
Sakaguchi,
K.
Wing,
Y.
Onishi,
P.
Prieto-Martin,
T.
Yamaguchi.
Regulatory T cells: how do they suppress immune responses?. International immunology.
2009;
21
:
1105-1111
.
-
S.
Sakaguchi,
T.
Yamaguchi,
T.
Nomura,
M.
Ono.
Regulatory T cells and immune tolerance. Cell.
2008;
133
:
775-787
.
-
D.
Sangiolo.
Cytokine induced killer cells as promising immunotherapy for solid tumors. Journal of Cancer.
2011;
2
:
363-368
.
-
F.C.
Schmeel,
L.C.
Schmeel,
S.M.
Gast,
I.G.
Schmidt-Wolf.
Adoptive immunotherapy strategies with cytokine-induced killer (CIK) cells in the treatment of hematological malignancies. International journal of molecular sciences.
2014;
15
:
14632-14648
.
-
L.C.
Schmeel,
F.C.
Schmeel,
C.
Coch,
I.G.
Schmidt-Wolf.
Cytokine-induced killer (CIK) cells in cancer immunotherapy: report of the international registry on CIK cells (IRCC). Journal of cancer research and clinical oncology.
2015;
141
:
839-849
.
-
J.
Schmidt,
S.
Eisold,
M.W.
Buchler,
A.
Marten.
Dendritic cells reduce number and function of CD4+CD25+ cells in cytokineinduced killer cells derived from patients with pancreatic carcinoma. Cancer.
2004;
immunology
:
immunotherapy : CII 53, 1018-1026
.
-
J.R.
Schoenborn,
C.B.
Wilson.
Regulation of interferongamma during innate and adaptive immune responses. Advances in immunology.
2007;
96
:
41-101
.
-
K.
Schroder,
P.J.
Hertzog,
T.
Ravasi,
D.A.
Hume.
Interferon-gamma: an overview of signals, mechanisms and functions. Journal of leukocyte biology.
2004;
75
:
163-189
.
-
S.
Sun,
X.M.
Li,
X.D.
Li,
W.S.
Yang.
Studies on inducing apoptosis effects and mechanism of CIK cells for MGC-803 gastric cancer cell lines. Cancer biotherapy & radiopharmaceuticals.
2005;
20
:
173-180
.
-
F.S.
Wang,
M.X.
Liu,
B.
Zhang,
M.
Shi,
Z.Y.
Lei,
W.B.
Sun,
Q.Y.
Du,
J.M.
Chen.
Antitumor activities of human autologous cytokine-induced killer (CIK) cells against hepatocellular carcinoma cells in vitro and in vivo. World journal of gastroenterology : WJG.
2002;
8
:
464-468
.
-
M.
Wang,
J.X.
Cao,
J.H.
Pan,
Y.S.
Liu,
B.L.
Xu,
D.
Li,
X.Y.
Zhang,
J.L.
Li,
J.L.
Liu,
H.B.
Wang.
Adoptive immunotherapy of cytokine-induced killer cell therapy in the treatment of nonsmall cell lung cancer. PloS one.
2014a;
9
:
e112662
.
-
M.
Wang,
S.B.
Shi,
J.L.
Qi,
X.Y.
Tang,
J.
Tian.
S-1 plus CIK as second-line treatment for advanced pancreatic cancer. Medical oncology.
2013a;
30
:
747
.
-
Q.J.
Wang,
H.
Wang,
K.
Pan,
Y.Q.
Li,
L.X.
Huang,
S.P.
Chen,
J.
He,
M.L.
Ke,
J.J.
Zhao,
J.J.
Li.
Comparative study on antitumor immune response of autologous cytokine-induced killer (CIK) cells, dendritic cells-CIK (DC-CIK), and semi-allogeneic DC-CIK. Chinese journal of cancer.
2010;
29
:
641-648
.
-
W.
Wang,
M.
Meng,
Y.
Zhang,
C.
Wei,
Y.
Xie,
L.
Jiang,
C.
Wang,
F.
Yang,
W.
Tang,
X.
Jin.
Global transcriptome-wide analysis of CIK cells identify distinct roles of IL-2 and IL-15 in acquisition of cytotoxic capacity against tumor. BMC medical genomics.
2014b;
7
:
49
.
-
Y.
Wang,
J.
Bo,
H.R.
Dai,
X.C.
Lu,
H.Y.
Lv,
B.
Yang,
T.
Wang,
W.D.
Han.
CIK cells from recurrent or refractory AML patients can be efficiently expanded in vitro and used for reduction of leukemic blasts in vivo. Experimental hematology.
2013b;
41
:
241-252 e243
.
-
Y.F.
Wang,
P.E.
Kunda,
J.W.
Lin,
H.
Wang,
X.M.
Chen,
Q.L.
Liu,
T.
Liu.
Cytokine-induced killer cells co-cultured with complete tumor antigen-loaded dendritic cells, have enhanced selective cytotoxicity on carboplatin-resistant retinoblastoma cells. Oncology reports.
2013c;
29
:
1841-1850
.
-
C.
Wei,
W.
Wang,
W.
Pang,
M.
Meng,
L.
Jiang,
S.
Xue,
Y.
Xie,
R.
Li,
Z.
Hou.
The CIK cells stimulated with combination of IL-2 and IL-15 provide an improved cytotoxic capacity against human lung adenocarcinoma. Tumour biology : the journal of the International Society for Oncodevelopmental Biology and Medicine.
2014;
35
:
1997-2007
.
-
X.C.
Wei,
X.H.
Zhai,
X.R.
Han,
D.D.
Yang,
Q.S.
Wang.
Influence of dendritic cells on biological activity of the homologous CIK cells and its anti-leukemia effect in vitro. Zhongguo shi yan xue ye xue za zhi /Zhongguo bing li sheng li xue hui = Journal of experimental hematology /Chinese Association of Pathophysiology.
2010;
18
:
946-951
.
-
X.C.
Wei,
X.H.
Zhai,
X.R.
Han,
D.D.
Yang,
W.L.
Zhao.
Biological activity of DC-CIK cells and its effect against leukemia cells in vitro. Zhongguo shi yan xue ye xue za zhi / Zhongguo bing li sheng li xue hui =Journal of experimental hematology / Chinese Association of Pathophysiology.
2008;
16
:
1150-1153
.
-
A.
Wongkajornsilp,
S.
Sangsuriyong,
S.
Hongeng,
S.
Waikakul,
A.
Asavamongkolkul,
S.
Huabprasert.
Effective osteosarcoma cytolysis using cytokine-induced killer cells pre-inoculated with tumor RNA-pulsed dendritic cells. Journal of orthopaedic research : official publication of the Orthopaedic Research.
2005;
Society23
:
1460-1466
.
-
L.
Yang,
B.
Ren,
H.
Li,
J.
Yu,
S.
Cao,
X.
Hao,
X.
Ren.
Enhanced antitumor effects of DC-activated CIKs to chemotherapy treatment in a single cohort of advanced non-small-cell lung cancer patients. Cancer.
2013;
immunology
:
immunotherapy : CII 62, 65-73
.
-
S.H.
Yoon,
J.M.
Lee,
S.J.
Woo,
M.J.
Park,
J.S.
Park,
H.S.
Kim,
M.Y.
Park,
H.J.
Sohn,
T.G.
Kim.
Transfer of Her-2/neu specificity into cytokine-induced killer (CIK) cells with RNA encoding chimeric immune receptor (CIR). Journal of clinical immunology.
2009;
29
:
806-814
.
-
Y.
Yuanying,
N.
Lizhi,
M.
Feng,
W.
Xiaohua,
Z.
Jianying,
Y.
Fei,
J.
Feng,
H.
Lihua,
C.
Jibing,
L.
Jialiang.
Therapeutic outcomes of combining cryotherapy, chemotherapy and DC-CIK immunotherapy in the treatment of metastatic non-small cell lung cancer. Cryobiology.
2013;
67
:
235-240
.
-
Y.
Zhang,
L.
Xia,
Y.
Zhang,
Y.
Wang,
X.
Lu,
F.
Shi,
Y.
Liu,
M.
Chen,
K.
Feng,
W.
Zhang.
Analysis of adverse events following the treatment of autologous cytokine-induced killer cells for adoptive immunotherapy in malignant tumour sufferers. Expert opinion on biological therapy.
2015;
15
:
481-493
.
-
Y.S.
Zhang,
F.J.
Yuan,
G.F.
Jia,
J.F.
Zhang,
L.Y.
Hu,
L.
Huang,
J.
Wang,
Z.Q.
Dai.
CIK cells from patients with HCC possess strong cytotoxicity to multidrug-resistant cell line Bel-7402/R. World journal of gastroenterology : WJG.
2005;
11
:
3339-3345
.
-
Q.
Zhao,
H.
Zhang,
Y.
Li,
J.
Liu,
X.
Hu,
L.
Fan.
Antitumor effects of CIK combined with oxaliplatin in human oxaliplatinresistant gastric cancer cells in vivo and in vitro. Journal of experimental & clinical cancer research : CR.
2010;
29
:
118
.
-
Y.J.
Zhao,
N.
Jiang,
Q.K.
Song,
J.P.
Wu,
Y.G.
Song,
H.M.
Zhang,
F.
Chen,
L.
Zhou,
X.L.
Wang,
X.N.
Zhou.
Continuous DC-CIK infusions restore CD8+ cellular immunity, physical activity and improve clinical efficacy in advanced cancer patients unresponsive to conventional treatments. Asian Pacific journal of cancer prevention : APJCP.
2015;
16
:
2419-242
.
Comments
Downloads
Article Details
Volume & Issue : Vol 3 No 03 (2016)
Page No.: 533-541
Published on: 2016-03-25
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 6630 times
- Download PDF downloaded - 1653 times
- View Article downloaded - 9 times
 Biomedpress
Biomedpress

