Abstract
Background: Anisometropia is a common refractive error. It has been associated with an increased risk of developing amblyopia, a condition that can lead to permanent vision loss if left untreated. This study aimed to systematically review and pool the available evidence on the relationship between anisometropia and amblyopia.
Methods: A systematic review and meta-analysis was conducted following the PRISMA guidelines. Three main databases were searched for observational studies that addressed the association between anisometropia and the risk of developing amblyopia. The quality of the included studies was assessed using the Newcastle–Ottawa scale.
Results: A total of 14 studies were included in the meta-analysis, with a combined sample size of 6,895 participants. Patients with any refractive error had a higher risk of developing amblyopia compared to those without refractive errors (P<0.05). However, the risk of developing amblyopia in patients with refractive errors of less than 1 diopter was relatively small (OR: 1.66, 95% CI: 1.2, 2.12).
Conclusion: This systematic review and meta-analysis provide evidence of a significant association between anisometropia and the risk of developing amblyopia. This highlights the importance of early detection and treatment of anisometropia as a potential strategy for preventing amblyopia.
Introduction
Amblyopia, or lazy eye, refers to the reduction of vision in one or both eyes without any ocular pathology1. This condition involves a decrease in best-corrected visual acuity in one or both eyes that is not related to any structural eye problems or visual pathway abnormalities2. The visual impairment caused by this disease can affect the visual cortex of the brain and disrupt cortical connections in various brain regions such as the frontal and parietal cortices during the critical period of brain development. This can lead to impairments in decision-making, response, and quality of life3. According to a meta-analysis study conducted in China in 2019, the prevalence of amblyopia was 1.44% globally: 1.09% in Asia, 2.44% in North America, and 2.90% in Europe. The highest prevalence was 3.29% in individuals over 20 years of age, with no gender differences. Based on that study, an estimated 99.2 million people worldwide are affected by amblyopia, which will increase to 175.2 million by 2030 and 221.9 million by 20404.
A systematic review study conducted in 2018 showed that the prevalence of this disease in Iran was 3.69%5. Another study conducted in Iran in 2018 indicated that the prevalence of amblyopia between 1990 and 2018 had decreased in the provinces of Hormozgan, Tehran, and Qom, but it increased in 13 other provinces6.
Anisometropia refers to the difference in refractive error between the two eyes, with a difference of equal to or greater than 1 diopter. The prevalence of anisometropia is less than 18% before the age of 40, and most studies show a prevalence of less than 10%. The prevalence of anisometropia appears to be age-dependent and higher in adults than in children. Mild anisometropia can be tolerated with special glasses, but degrees greater than 4 diopters are susceptible to progressing toward amblyopia7. According to a meta-analysis study conducted in 2018, the global prevalence of amblyopia was 1.75%8.
Recognizing the risk factors of amblyopia and timely prevention and treatment can prevent visual impairment and improve quality of life. Several studies have been conducted on the relationship between anisometropia and the risk of developing amblyopia. Some have shown a significant relationship between the two, whereas others have found no significant association. Since no comprehensive meta-analysis study has been conducted to determine the relationship between these two diseases, this study aimed to investigate the relationship between anisometropia and amblyopia through a systematic review and meta-analysis of similar studies.
Methods
This article presents a systematic review and meta-analysis conducted to investigate the relationship between anisometropia and amblyopia. The systematic review methodology was developed using the checklist of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)9.
The study population included all patients with both amblyopia and anisometropia, without restrictions on age, gender, or race. Relevant studies on the relationship between anisometropia and the important risk factor of amblyopia were extracted from three main databases, Scopus, ISI Web of Science, and PubMed, from their inception until February 2022. They were entered into the meta-analysis by related keywords including “anisometropia,” “amblyopia,” and “reflective error”. All observational studies (cohort, case-control, and cross-sectional) that addressed the relationship between amblyopia and anisometropia were included in this meta-analysis, regardless of language, time frame, or publication status. To identify additional potential studies of interest, the reference lists of the selected articles were evaluated. The inclusion criteria were all studies that mentioned the outcome of amblyopia and exposure to anisometropia. The exclusion criteria were qualitative studies, editorials, case reports, case series, and review studies.
The electronic data collection form was designed to extract the necessary data, including the first author’s name, year of publication, country, study type, patient occupational group, mean age of patients, study type, sample size in the intervention and control groups, diagnostic criteria for amblyopia, and odds ratio (OR) in both crude and adjusted forms. The data extraction was completed by two independent reviewers (SK and TM).
The methodological quality of the studies was assessed based on the Newcastle–Ottawa and Ottawa Statement guidelines. These guidelines include criteria for selecting study participants, comparability, and exposure and outcome considerations, with a maximum of nine stars assigned to each study. Studies with seven or more stars were considered high-quality studies, and studies with six or fewer stars were classified as low-quality studies. The possibility of bias in the study results was separately assessed by two researchers, and any disagreement was resolved through discussion.
The effect of anisometropia on amblyopia was expressed in terms of OR with a 95% confidence interval (CI). The I2 statistic was calculated to evaluate the heterogeneity among the studies. For all analyses, a random effect model was reported. Stata 14 software was used to analyze the data.
| First Author | Year | Study-design | Country | Sample size | Characteristics | Magnitude of Anisometropia | Adjusted | OR (95%CI) |
|---|---|---|---|---|---|---|---|---|
| Leon et al . 10 | 2008 | Retrospective observational study | USA | 974 | Mean age: 3.7 year (Range: 0-6) | 2-4D vs. 1-2D >4D vs. 2-4D | - | 2.13 (1.63, 2.78] 2.34 (1.67, 3.28] |
| Pai, Amy Shih-I et al . 11 | 2011 | Population-based, cross-sectional study | Australia | 1422 | 30 to 72 months | ≥ 1D | age, gender, and ethnicity | 27.82 (11.17-69.31) |
| Huynh et al . 12 | 2015 | population based study | Australia | 1724 | Mean age: 6.7±0.4 year Boys: 50.7% | - | worse eye refraction, multiple birth and strabismus | 29.3 (8.7 to 99) |
| Borchert et al . 13 | 2009 | Population-based, cross-sectional study | USA | 6024 | Age: 6 to 72 months Race: Hispanic and African American children | Spherical and cylindrical anisometropia (1.0 D) | age, gender, and ethnicity | Family amblyopia 3.5 (1.22–10.03 ) |
| Ying, Gui-shuang et al . 14 | 2013 | Multicenter, cross-sectional study | USA | 3728 | 3-5 year old ages | SE: Any 0.25 D >0.25-0.5D >0.5, 0.75D >0.75-1.75D >1.75-12.3D | - | 3.34 (2.12–5.26) 0.78 (0.34-1.82) 1.52 (0.81–2.88) 4.89 (2.44-9.81) 11.5 (6.37-20.8) 41.7 (20.7-84.1) |
| Meng et al. 15 | 2020 | A cross-sectional study | China | 1852 | Age: 6.83 ± 0.46 | SE ≥0 to <+0.50 D ≥+0.50 to<+1.00 D ≥+1.00 | all the other refractive risk factors | Ref 3.95 (1.44–10.79) 21.90 (8.24–58.18) |
| Mocanu et al . 16 | 2018 | cross-sectional study | Romania | 1231 | Age: 5-16 years | Anisometropia | - | 119.2 (35–405.91) |
| Dan Huang et al . 17 | 2018 | population-based cross-sectional, study | China | 1695 | children aged 36–48 months | SE anisometropia <1.00 ≥1.00 to <2.00 ≥2.0 | other refractive risk factors | Ref 2.87 (0.73 - 11.27) 5.87 (1.52 - 22.77) |
| Pascual, Maisie et al . 18 | 2013 | Multicenter, cross-sectional study | USA | 3869 | 36-72 months of age | 0.5 and <1.0D 1.0 and <2.0D >2.0D | other refractive risk factors | 1.65 (1.21-2.26) 4.26 (2.79-6.51) 9.16 (4.96-16.9) |
| Robaei 19 | 2006 | population-based survey | Australia | 1740 | mean age: 6.7 years (range, 5.5-8.4 years) Boys: 50.6% | Anisometropia >1D | 156 (64–382) | |
| Chia et al . 20 | 2013 | population-based cross-sectional | Singapore | 2015 | Race: Chinese Age: 30–72 months | >1D | adjusting for age, sex, past admission to a NICU, socioeconomic factors, maternal age, prematurity and maternal smoking | 20.65 (4.65- 91.75) |
| Afsari et al . 21 | 2014 | population-based survey | Australia | 2090 | aged 6–72 months | SE anisometropia ≥1D ≥1.5D ≥2.0D | Age | 12.4 (4.0 to 38.4) 18.7 (4.1 to 84.5) 33.2 (6.32 to 179) |
| Gursoy et al . 22 | 2013 | population-based cross-sectional | Turkey | 709 | Age: 7-8 year Boys: 51% | ≥1D | - | 6.32 (3–13.33) |
| Fu et al . 23 | 2013 | cross-sectional study | China | 3112 | Mean age: 7.1±0.4 years | Anisometropia | - | 26.08 (10.93–62.21 |
| Any diopter | Less than one diopter | Between one to two diopters | Greater than one diopter | Greater than two diopter | |
| Crude OR | 4.78 (0, 9.81) | 1.66 (1.2, 2.12) | 4.26 (2.4, 6.12) | 10.44 ( 3.57, 23.93) | 9.75 ( 4.57, 14.9) |
| Adjusted OR | 3.38 (1.91, 4.86) | 4.01 (0.25, 7.77) | 6.81 (0, 6.12) | 17.49 (6.28, 28.71) | 20.82 ( 0, 49.28) |
| Overal OR | 3.17 (1.87, 4.47) | 1.63 (1.15, 2.09) | 14.6 (5.99, 23.24) | 14.62 (5.99, 23.24) | 9.81 ( 5.08, 14.55) |
| n. of studies | 6 | 4 | 3 | 5 | 6 |
| I2 | 0.18 | 0.67 | 0.13 | 0.81 | 0.4 |
Results
In the initial search, a total of 3,840 articles were obtained. Of these, 3,621 were retrieved from the electronic databases up to February 2022, and 219 were identified through hand searching. Using EndNote software, 700 duplicate articles were detected and removed, and after screening the titles and abstracts, 2,824 articles that were not relevant to the objectives of this study were excluded. Consequently, 100 articles were selected for full-text review, of which 86 did not meet the inclusion criteria of this study and were excluded. Finally, 14 studies were included in the meta-analysis (Figure 1), which consisted of 40,963 participants in total. All were cross-sectional studies published in English.
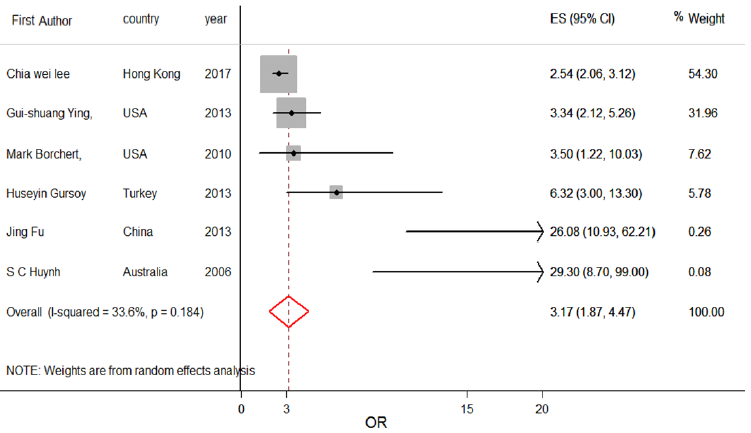
Figure 2 shows the association between refractive errors of any magnitude and the risk of developing amblyopia. In patients with refractive errors of any magnitude, the risk of developing amblyopia was 3.17 times higher (OR: 3.17, 95% CI: 1.87, 4.47). Subgroup analysis showed that the association between refractive errors of any magnitude and the risk of developing amblyopia was not significant in a crude analysis (OR: 4.78, 95% CI: 0, 9.81), but the results of the adjusted model showed a significant association (OR: 3.38, 95% CI: 1.91, 4.86). This means that individuals with any refractive error had a 3.38 times greater chance of developing amblyopia compared to those without refractive errors, after adjusting for potential confounding factors.
Figure 3 shows the association between refractive errors of less than 1 diopter and the risk of developing amblyopia. In patients with refractive errors of less than 1 diopter, the risk of developing amblyopia was 1.66 times higher (OR: 1.66, 95% CI: 1.2, 2.12). Subgroup analysis showed that the association between refractive errors of less than 1 diopter and the risk of developing amblyopia was not significant in a crude analysis (OR: 4.01, 95% CI: 0.25, 7.77), but the results of the adjusted model showed a significant association (OR: 1.63, 95% CI: 1.15, 2.09). This means that individuals with refractive errors of zero to 1 diopter had a 1.623 times greater chance of developing amblyopia compared to those without refractive errors.
Figure 4 shows the association between refractive errors between one to two diopters and the risk of developing amblyopia. In patients with refractive errors of 1–2 diopters, the risk of developing amblyopia was 14.62 times higher (OR: 14.62, 95% CI: 5.99, 23.24). Subgroup analysis showed that the association between refractive errors of greater than 1 diopter and the risk of developing amblyopia was significant in a crude analysis (OR: 4.26, 95% CI: 2.4, 6.12), but the results of the adjusted model did not show a significant association (OR: 6.81, 95% CI: 0, 6.12).
Figure 5 shows the association between refractive errors greater than 1 diopter and the risk of developing amblyopia. In patients with refractive errors of greater than 1 diopter, the risk of developing amblyopia was 14.62 times higher (OR: 14.62, 95% CI: 5.99, 23.24). Subgroup analysis showed that the association between refractive errors of greater than 1 diopter and the risk of developing amblyopia was not significant in a crude analysis (OR: 10.44, 95% CI: 0, 23.93), but the results of the adjusted model showed a significant association (OR: 17.49, 95% CI: 6.28, 28.71).
Figure 6 shows the association between refractive errors of greater than 2 diopters and the risk of developing amblyopia. In patients with refractive errors of greater than 2 diopters, the risk of developing amblyopia was 9.81 times higher (OR: 9.81, 95% CI: 5.08, 14.55). Subgroup analysis showed that the association between refractive errors of greater than 2 diopters and the risk of developing amblyopia was significant in a crude analysis (OR: 9.75, 95% CI: 4.57, 14.9), but the results of the adjusted model did not show a significant association (OR: 20.82, 95% CI: 0, 49.28).
All the studies included in this meta-analysis were judged to be high-quality based on the NOS. The overall study results are presented in Table 2.
Discussion
In this review study, we examined the available evidence from epidemiological studies that had identified the association between anisometropia and the risk of developing amblyopia. This is the first such meta-analysis conducted, and the main findings suggest a significant association between refractive errors and the risk of developing amblyopia. Patients with any refractive error had a higher risk of developing amblyopia compared to those without refractive errors. However, the risk of developing amblyopia in patients with refractive errors of less than 1 diopter was relatively small.
The findings of this study will be useful in implementing various programs for preventing the development of amblyopia among children. Children with anisometropic-type amblyopia are usually diagnosed later than children with other types, likely because of the lack of significant physical abnormalities in these children, unlike those with strabismus who typically have an obvious problem that is easily diagnosed.
The American Association for Pediatric Ophthalmology and Strabismus has established certain criteria for diagnosing refractive errors that should be identified through preschool vision screening if they exceed 1.5 diopters24. However, these criteria are likely too strict since low levels of anisometropia do not seem to cause significant amblyopia in young children and are easily treatable. Therefore, a review is needed to recommend diagnosis only when the degree of anisometropia exceeds 2 diopters in children under 3 years of age since our study indicated no significant relationship between anisometropia and amblyopia at 1–2 diopters.
Infants may have a threshold of up to 3 diopters for developing anisometropic amblyopia, as shown by Abrahamsson and Sjöstrand25. By adopting a higher standard, the referral rate, false-positive rate, and overall cost of screening programs can be significantly reduced. Higher target levels may even be appropriate for field screenings that require a very high level of specificity. However, being overly sensitive to risk may result in some children with mild to moderate amblyopia not receiving treatment and progressing toward more severe levels, which can make final treatment more challenging and increase the likelihood of recurrence26.
Leon et al. conducted a retrospective study in the United States in 2008, which found a correlation between anisometropia and amblyopia. The study indicated that as the severity of anisometropia increased, the likelihood of developing amblyopia also increased. Specifically, the odds of developing amblyopia increased to 2.13 (95% CI: 1.63, 2.78) with 2–4 diopters and 2.34 (95% CI: 1.67, 3.2) with 4 diopters or greater, compared to 1–2 diopters. These findings are consistent with those of the present study and support the notion that an increase in the severity of anisometropia is associated with an increased risk of developing amblyopia10.
If anisometropia is identified and treated early, the likelihood of developing amblyopia decreases. Anisometropia should be screened regularly and in the early stages to identify it. If anisometropia is detected, using suitable glasses or lenses may be necessary to balance the stimulation between the two eyes and reduce the risk of developing amblyopia. In more severe cases, surgery may be required. Therefore, early identification and treatment of anisometropia can help prevent amblyopia and is essential for maintaining and improving children’s vision.
Some potential limitations of the study exist. First, the included studies may have differences in terms of patient characteristics and diagnostic criteria, which could result in heterogeneity in the results. Secondly, the study relied on the adjusted effect estimates reported in the included studies, but unmeasured confounding factors such as age group that were not considered in the analysis are possible.
Conclusion
Patients with anisometropia had a higher risk of developing amblyopia compared to those without anisometropia. This study highlights the importance of early detection and treatment of anisometropia as a potential strategy for preventing amblyopia.
Abbreviations
CI: Confidence interval, PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses, OR: Odds ratio
Acknowledgments
The authors would like to express their gratitude to the Vice-Chancellor of the Research and Technology from Hamadan University of Medical Sciences who financially supported the project (Research Id: 140010289091, Ethics code: IR.UMSHA.REC.1400.834).
Author’s contributions
All authors read and approved the final manuscript.
Funding
Hamadan University of Medical Sciences who financially supported the project (Research Id: 140010289091, Ethics code: IR.UMSHA.REC.1400.834).
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Quoc
E.B.,
Kulp
M.T.,
Burns
J.G.,
Thompson
B.,
Amblyopia - A review of unmet needs, current treatment options, and emerging therapies. Survey of Ophthalmology.
2023;
68
(3)
:
507-525
.
View Article Google Scholar -
Rubin
S.E.,
Nelson
L.B.,
Amblyopia. Diagnosis and management. Pediatric Clinics of North America.
1993;
40
(4)
:
727-35
.
View Article PubMed Google Scholar -
Farzin
F.,
Norcia
A.M.,
Impaired visual decision-making in individuals with amblyopia. Journal of Vision (Charlottesville, Va.).
2011;
11
(14)
:
6
.
View Article PubMed Google Scholar -
Fu
Z.,
Hong
H.,
Su
Z.,
Lou
B.,
Pan
C.W.,
Liu
H.,
Global prevalence of amblyopia and disease burden projections through 2040: a systematic review and meta-analysis. The British Journal of Ophthalmology.
2020;
104
(8)
:
1164-70
.
View Article PubMed Google Scholar -
Chegeni
M.,
Khanjani
N.,
Rahmatpour
P.,
Ahmadi Pishkuhi
M.,
Abdolalian
N.,
The prevalence of amblyopia in Iran: A systematic review. Journal of Current Ophthalmology.
2018;
30
(3)
:
194-201
.
View Article PubMed Google Scholar -
Ashrafi
E.,
Jamali
S.,
Mohammadi
S.F.,
Mehdipoor
P.,
National and sub national prevalence of Amblyopia and its trends from 1990 to 2018 in Iran. Journal of Optometry.
2020;
13
(2)
:
113-9
.
View Article PubMed Google Scholar -
Zedan
R.H.,
El-Fayoumi
D.,
Awadein
A.,
Progression of high anisometropia in children. Journal of Pediatric Ophthalmology and Strabismus.
2017;
54
(5)
:
282-6
.
View Article PubMed Google Scholar -
Hashemi
H.,
Pakzad
R.,
Yekta
A.,
Bostamzad
P.,
Aghamirsalim
M.,
Sardari
S.,
Global and regional estimates of prevalence of amblyopia: A systematic review and meta-analysis. Strabismus.
2018;
26
(4)
:
168-83
.
View Article PubMed Google Scholar -
Moher
D.,
Shamseer
L.,
Clarke
M.,
Ghersi
D.,
Liberati
A.,
Petticrew
M.,
Group
PRISMA-P,
Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews.
2015;
4
(1)
:
1-9
.
View Article PubMed Google Scholar -
Borchert
M.,
Tarczy-Hornoch
K.,
Cotter
S.A.,
Liu
N.,
Azen
S.P.,
Varma
R.,
Anisometropia in Hispanic and African American infants and young children: The multi-ethnic pediatric eye disease study. Ophthalmology.
2010;
117
(1)
:
148-53. e1
.
View Article Google Scholar -
Ying
G.S.,
Huang
J.,
Maguire
M.G.,
Quinn
G.,
Kulp
M.T.,
Ciner
E.,
Vision in Preschoolers Study Group
Associations of anisometropia with unilateral amblyopia, interocular acuity difference, and stereoacuity in preschoolers. Ophthalmology.
2013;
120
(3)
:
495-503
.
View Article PubMed Google Scholar -
Meng
Z.,
Fu
J.,
Chen
W.,
Li
L.,
Su
H.,
Dai
W.,
Prevalence of amblyopia and associated risk factors in Tibetan grade one children. Ophthalmic Research.
2021;
64
(2)
:
280-9
.
View Article PubMed Google Scholar -
Mocanu
V.,
Horhat
R.,
Prevalence and risk factors of amblyopia among refractive errors in an Eastern European population. Medicina (Kaunas, Lithuania).
2018;
54
(1)
:
6
.
View Article PubMed Google Scholar -
Huang
D.,
Chen
X.,
Zhu
H.,
Ding
H.,
Bai
J.,
Chen
J.,
Prevalence of amblyopia and its association with refraction in Chinese preschool children aged 36-48 months. The British Journal of Ophthalmology.
2018;
102
(6)
:
767-71
.
View Article PubMed Google Scholar -
Pascual
M.,
Huang
J.,
Maguire
M.G.,
Kulp
M.T.,
Quinn
G.E.,
Ciner
E.,
Risk factors for amblyopia in the vision in preschoolers study. Ophthalmology.
2014;
121
(3)
:
622-9. e1
.
View Article Google Scholar -
Robaei
D.,
Rose
K.A.,
Ojaimi
E.,
Kifley
A.,
Martin
F.J.,
Mitchell
P.,
Causes and associations of amblyopia in a population-based sample of 6-year-old Australian children. Archives of Ophthalmology.
2006;
124
(6)
:
878-84
.
View Article PubMed Google Scholar -
Chia
A.,
Lin
X.,
Dirani
M.,
Gazzard
G.,
Ramamurthy
D.,
Quah
B.L.,
Risk factors for strabismus and amblyopia in young Singapore Chinese children. Ophthalmic Epidemiology.
2013;
20
(3)
:
138-47
.
View Article PubMed Google Scholar -
Leon
A.,
Donahue
S.P.,
Morrison
D.G.,
Estes
R.L.,
Li
C.,
The age-dependent effect of anisometropia magnitude on anisometropic amblyopia severity. Journal of AAPOS.
2008;
12
(2)
:
150-6
.
View Article PubMed Google Scholar -
Gursoy
H.,
Basmak
H.,
Yaz
Y.,
Colak
E.,
Vision screening in children entering school: Eskisehir, Turkey. Ophthalmic Epidemiology.
2013;
20
(4)
:
232-8
.
View Article PubMed Google Scholar -
Fu
J.,
Li
S.M.,
Li
S.Y.,
Li
J.L.,
Li
H.,
Zhu
B.D.,
Prevalence, causes and associations of amblyopia in year 1 students in Central China : the Anyang childhood eye study (ACES). Graefe's Archive for Clinical and Experimental Ophthalmology .
2014;
252
(1)
:
137-43
.
View Article PubMed Google Scholar -
Pai
A.S.,
Rose
K.A.,
Leone
J.F.,
Sharbini
S.,
Burlutsky
G.,
Varma
R.,
Amblyopia prevalence and risk factors in Australian preschool children. Ophthalmology.
2012;
119
(1)
:
138-44
.
View Article PubMed Google Scholar -
Huynh
S.C.,
Wang
X.Y.,
Ip
J.,
Robaei
D.,
Kifley
A.,
Rose
K.A.,
Prevalence and associations of anisometropia and aniso-astigmatism in a population based sample of 6 year old children. The British Journal of Ophthalmology.
2006;
90
(5)
:
597-601
.
View Article PubMed Google Scholar -
Afsari
S.,
Rose
K.A.,
Gole
G.A.,
Philip
K.,
Leone
J.F.,
French
A.,
Prevalence of anisometropia and its association with refractive error and amblyopia in preschool children. The British Journal of Ophthalmology.
2013;
97
(9)
:
1095-9
.
View Article PubMed Google Scholar -
Arnold
R.W.,
Donahue
S.P.,
Silbert
D.I.,
Longmuir
S.Q.,
Bradford
G.E.,
Peterseim
M.M.W.,
AAPOS uniform guidelines for instrument-based pediatric vision screen validation 2021. Journal of American Association for Pediatric Ophthalmology and Strabismus.
2022;
26
(1)
:
1. e-e6
.
View Article Google Scholar -
Abrahamsson
M.,
Sjöstrand
J.,
Natural history of infantile anisometropia. The British Journal of Ophthalmology.
1996;
80
(10)
:
860-3
.
View Article PubMed Google Scholar -
Bradfield
Y.S.,
Identification and treatment of amblyopia. American Family Physician.
2013;
87
(5)
:
348-52
.
PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 10 No 11 (2023)
Page No.: 6009-6018
Published on: 2023-11-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 4245 times
- PDF downloaded - 1247 times
- XML downloaded - 98 times
 Biomedpress
Biomedpress







