Abstract
Background: Esophageal squamous cell carcinoma (ESCC) is a highly aggressive malignancy with a propensity for metastatic spread. Metastasis to the thyroid gland is a rare occurrence, with few reported cases in the literature. This report presents a rare case of advanced ESCC with metastases to the thyroid and supraclavicular lymph node, highlighting the importance of considering metastatic disease in patients with unusual thyroid lesions and a history of ESCC.
Case Presentation: A 68- year-old male with a history of cerebrovascular accident, tobacco use, and alcohol consumption presented with a progressively enlarging neck mass, dysphagia, and weight loss. Examinations revealed a pharyngeal mass, a suspicious thyroid lesion, and an abnormal left supraclavicular lymph node. Biopsies confirmed primary ESCC with metastases to the thyroid and left supraclavicular lymph node. Immunohistochemistry played a crucial role in confirming the esophageal origin of the metastatic lesions.
Conclusion: This case underscores the importance of thoroughly evaluating unusual thyroid lesions to rule out rare secondary malignancies, such as ESCC metastasis. A comprehensive diagnostic workup and a multidisciplinary approach are essential for accurate staging and optimal management in such cases. Clinicians should maintain a high index of suspicion for metastatic disease in patients with a history of ESCC presenting with thyroid nodules or masses. Early detection and close monitoring of suspicious thyroid lesions may improve patient outcomes, despite the generally poor prognosis associated with metastatic ESCC.
Introduction
Esophageal squamous cell carcinoma (ESCC) is a highly aggressive malignancy with a poor prognosis, often presenting at an advanced stage with metastatic spread1. ESCC is the predominant histological subtype of esophageal cancer, accounting for approximately 85% of cases worldwide2. Despite advances in diagnosis and treatment, the 5-year survival rate for ESCC remains low, ranging from 10% to 20%2.
Metastatic spread of ESCC to distant organs is a common occurrence, with the liver, lungs, and bones being the most frequently affected sites3. However, metastasis to the thyroid gland is extremely rare, estimated to occur in only 0.5-1.5% of thyroid metastases4, 5. Comprehensive reviews reveal that thyroid metastasis from ESCC typically presents in advanced-stage disease, with a median age of around 60 years and a slight male predominance6, 7. Previously reported cases of ESCC with concurrent thyroid and supraclavicular lymph node involvement are extremely rare. While there have been documented instances of supraclavicular lymph node metastasis in ESCC, specific cases involving both the thyroid and supraclavicular lymph nodes are limited8, 9, 10, making our case particularly unique. The mechanism of metastasis likely involves lymphatic spread, given the anatomical proximity and lymphatic drainage patterns between the esophagus and thyroid gland11. The proposed protective mechanisms of the thyroid include high oxygen saturation and iodine concentration of venous blood, which may hinder the adhesion and growth of tumor emboli12, 13, fast arterial flow impeding tumor adhesion14, and the thyroid capsule acting as a physical barrier15.
We report a rare case of advanced ESCC metastasizing to the thyroid and supraclavicular lymph nodes in a 68-year-old male. This case highlights the need for careful evaluation of unusual thyroid lesions to rule out secondary malignancies, especially in patients with a history of ESCC. It also demonstrates the necessity of comprehensive diagnostic workup and a multidisciplinary approach when assessing rare metastases. The aim of this report is to expand the limited evidence on this uncommon manifestation of ESCC and its aggressive course.
Case presentation
Patient History
A 68-year-old male with a history of cerebrovascular accident, which occurred a decade ago and from which he recovered without sequelae, presented to Hospital 1 with a chief complaint of a progressively enlarging neck mass. The patient reported associated symptoms of dysphagia and a sensation of fullness in the neck, which had been worsening over the past month, accompanied by unintentional weight loss. His past medical history was significant for heavy tobacco use, approximately one pack per day for 20 years, which ceased following his stroke. He also had a history of heavy alcohol consumption, which had been reduced significantly in the past decade.
Initial Evaluation and Referral
An initial evaluation at a private clinic suggested gastroesophageal reflux disease, and outpatient medication was prescribed with no improvement in symptoms. Upon further evaluation at Hospital 2, a magnetic resonance imaging (MRI) scan revealed a mass in the pharyngeal region (Figure 1). The patient was then referred to Hospital 3, where a thyroid mass was detected, leading to a subsequent referral to Hospital 1 for specialized assessment.
Diagnostic Workup
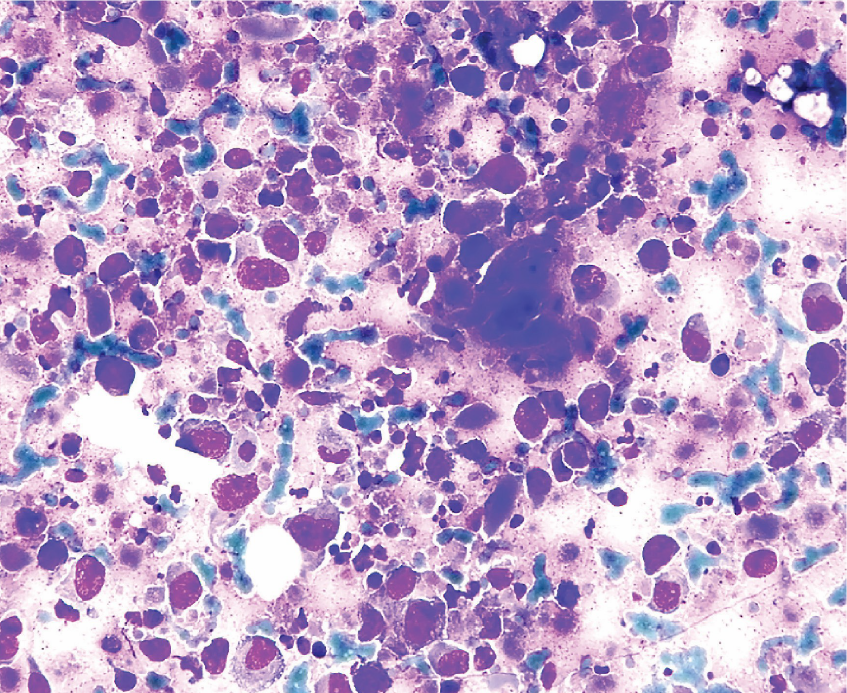
At Hospital 1, routine blood tests, including thyroid function tests (TFTs), were within normal limits. An ultrasound of the thyroid gland revealed a solid, hypoechoic nodule with irregular margins, microcalcifications, and increased vascularity in the left thyroid lobe, suggestive of malignancy (Figure 2 A). An ultrasound-guided fine-needle aspiration (FNA) of the left thyroid lobe lesion was performed. The cytological analysis showed abundant atypical squamous cells with enlarged, pleomorphic nuclei, prominent nucleoli, and dense cytoplasm, along with background keratin debris (Figure 2 B). Notably, no thyroid follicular cells were observed. The findings were consistent with metastatic squamous cell carcinoma and corresponded to Bethesda category V (suspicious for malignancy).
Gastrointestinal endoscopy identified an ulcerated, fungating lesion in the middle third of the esophagus, extending approximately 5 cm in length. Biopsy of the esophageal mass confirmed invasive squamous cell carcinoma (Figure 3). An abnormal lymph node in the left supraclavicular fossa was also identified and sampled, revealing metastatic squamous cell carcinoma, likely of esophageal origin (Figure 4).
Immunohistochemical Analysis
Immunohistochemical staining of the esophageal biopsy was negative for thyroid transcription factor-1 (TTF1) and thyroglobulin, confirming the primary origin of the tumor in the esophagus.
Diagnosis and Outcome
The patient was diagnosed with advanced-stage primary esophageal squamous cell carcinoma (ESCC) with metastases to the left thyroid lobe and left supraclavicular lymph node. Due to the rapid decline in the patient's health, no treatment was initiated, and the patient passed away approximately one month after the diagnosis.
Results
The case of a 68-year-old male diagnosed with advanced-stage primary ESCC with metastases to the left thyroid lobe and left supraclavicular lymph node is a rare occurrence, with thyroid metastases from distant primary tumors reported in only 1.4% to 3% of clinical series and up to 24% in autopsy studies16. The most common primary tumors metastasizing to the thyroid gland are renal cell carcinoma, lung cancer, and breast cancer17. Metastases from gastrointestinal tumors, including ESCC, to the thyroid gland are even rarer18.
Differentiating primary thyroid squamous cell carcinoma from metastatic ESCC is challenging and requires identifying the primary ESCC site5, 19. Although primary thyroid squamous cell carcinoma is rare, it should be considered in the differential diagnosis, particularly in patients with a history of smoking and alcohol consumption. In this case, the presence of a pharyngeal mass on imaging and endoscopy raises the possibility of hypopharyngeal squamous cell carcinoma extending to the thyroid gland, which is not uncommon. Immunohistochemistry was crucial, showing negative thyroid transcription factor-1 and thyroglobulin, confirming esophageal origin. In this case, several factors strongly suggest that the thyroid lesion is a metastasis from the primary ESCC, including the absence of thyroid follicular cells in the FNA sample, the patient's advanced-stage ESCC with confirmed metastasis to the left supraclavicular lymph node, and the rapid clinical deterioration and short survival time20, 21. Immunohistochemical markers, such as TTF-1, thyroglobulin, and PAX8, are useful in distinguishing between primary thyroid tumors and metastatic lesions22, 23. The absence of these markers in the present case further supports the diagnosis of metastatic ESCC to the thyroid gland.
The prognosis of patients with thyroid metastases from ESCC is particularly unfavorable24, with a reported median survival of 5-8 months4, 5. Early detection and close monitoring of suspicious thyroid lesions are crucial, and a high index of suspicion for metastatic disease should be maintained in patients with a history of ESCC presenting with thyroid nodules or masses. Prompt diagnostic workup and close collaboration between clinicians, radiologists, and pathologists are essential for accurate diagnosis and staging. There is no clear consensus on diagnostic criteria and management, but reported options include thyroidectomy, chemotherapy, radiation, or combined modalities, albeit with limited efficacy4, 5, 25. The choice of treatment depends on factors such as the primary tumor type, the extent of metastatic disease, and the patient's overall health and prognosis26. In cases of advanced-stage cancer with multiple metastases and poor performance status, as in the present case, palliative care may be the most appropriate approach to improve quality of life27.
The findings from this case have several important implications for clinical practice and future research. First, the presence of thyroid metastasis in ESCC may serve as an indicator of particularly aggressive disease requiring urgent intervention10. Second, the concurrent involvement of supraclavicular lymph nodes suggests a potential metastatic pathway that warrants further investigation28. From a diagnostic perspective, our case emphasizes the importance of comprehensive immunohistochemical analysis in distinguishing primary thyroid malignancies from metastatic disease29. Future research directions should focus on: (1) developing predictive models for unusual metastatic patterns in ESCC, (2) investigating the role of novel imaging techniques in early detection of thyroid metastasis, and (3) evaluating the efficacy of targeted therapies in such cases.
While genetic testing was not performed in this case due to rapid disease progression and limited clinical utility in the terminal stage, we acknowledge this limitation. Recent studies have identified several genetic alterations associated with ESCC metastasis, including mutations in TP53, PIK3CA, and NOTCH1 genes, as well as dysregulation of various molecular pathways such as WNT/β-catenin and PI3K/AKT/mTOR signaling30, 31, 32. Additionally, specific biomarkers like PTEN, STMN1, and TNFAIP8 have been linked to ESCC metastatic potential33. Future studies should aim to identify specific genetic alterations or biomarkers that may predict the risk of metastasis and guide personalized treatment strategies, particularly focusing on rare metastatic sites such as the thyroid gland34.
While our patient's rapid decline precluded active treatment, several therapeutic options merit consideration for similar cases. For isolated thyroid metastasis, surgical resection may be considered in selected patients with good performance status14. Systemic therapy options for metastatic ESCC include platinum-based chemotherapy combinations35. Recent advances in immunotherapy, particularly immune checkpoint inhibitors, have demonstrated promising results in advanced ESCC36. Palliative radiotherapy may provide local control and symptom relief, particularly for dysphagia37. The choice of treatment should be individualized based on patient factors, disease extent, and molecular profile when available.
Conclusions
The case report highlights the rare occurrence of metastatic esophageal squamous cell carcinoma (ESCC) in the thyroid gland and the diagnostic challenges it presents. The current case aims to raise awareness among clinicians about the possibility of ESCC metastasis in the differential diagnosis of unusual thyroid lesions, especially in patients with a history of ESCC. A comprehensive diagnostic approach, including imaging studies, fine-needle aspiration, and immunohistochemical staining, is essential for accurate diagnosis and staging. The aggressive nature of metastatic ESCC to the thyroid gland underscores the importance of early detection and close monitoring of suspicious thyroid lesions in patients with a history of ESCC. A multidisciplinary approach involving clinicians, radiologists, and pathologists is crucial for optimal patient management. This case emphasizes the need for heightened awareness among various clinicians beyond oncologists and endocrinologists, including general practitioners and head and neck surgeons, and highlights the necessity for future research in this area.
Abbreviations
AJCC: American Joint Committee on Cancer, ESCC: Esophageal Squamous Cell Carcinoma, FNA: Fine-Needle Aspiration, MRI: Magnetic Resonance Imaging, NOTCH1: Notch Receptor 1, PET/CT: Positron Emission Tomography/Computed Tomography, PI3K/AKT/mTOR: Phosphoinositide 3-Kinase / Protein Kinase B (AKT) / Mammalian Target of Rapamycin, PIK3CA: Phosphatidylinositol-4,5-Bisphosphate 3-Kinase Catalytic Subunit Alpha, PTEN: Phosphatase and Tensin Homolog, STMN1: Stathmin 1, TFTs: Thyroid Function Tests, TNFAIP8: Tumor Necrosis Factor Alpha-Induced Protein 8, TP53: Tumor Protein p53, TTF1: Thyroid Transcription Factor-1, UICC: Union for International Cancer Control, WNT/β-catenin: Wnt Signaling Pathway / Beta-Catenin
Acknowledgments
None.
Author’s contributions
DVN and CTD conceived the study and participated in its design and coordination. DVN, HTD, THD, and DQV participated in data curation and investigation. DVN and CTD drafted the manuscript. HTD, THD, and DQV critically revised the manuscript for important intellectual content. CTD supervised the study and provided methodological guidance. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This case report was conducted in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The article is written according to the guidelines of the ethics committee of our institution. This case report was exempt from formal ethical approval at our institution as it involved only retrospective review of medical records and did not involve any direct patient contact or intervention. All patient information has been sufficiently anonymized to protect the patient's identity and confidentiality.
Consent for publication
Written informed consent was obtained from the patient's next of kin for publication of this case report and any accompanying images, as the patient had passed away shortly after the diagnosis. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
References
-
Tian
D.,
Jiang
K.Y.,
Yang
Y.S.,
Yan
H.J.,
Yu
R.X.,
Huang
H.,
Pararespiratory and paradigestive lymph node metastases in esophageal squamous cell carcinoma: predicting survival and refining the N staging system. BMC Cancer.
2023;
23
(1)
:
695
.
View Article PubMed Google Scholar -
Wei
D.D.,
Fang
J.M.,
Wang
H.Z.,
Chen
J.,
Kong
S.,
Jiang
Y.Y.,
Perioperative immunotherapy for esophageal squamous cell carcinoma. Frontiers in Immunology.
2024;
15
:
1330785
.
View Article PubMed Google Scholar -
Waters
J.K.,
Reznik
S.I.,
Update on Management of Squamous Cell Esophageal Cancer. Current Oncology Reports.
2022;
24
(3)
:
375-85
.
View Article PubMed Google Scholar -
Zhang
X.,
Gu
X.,
Li
J.G.,
Hu
X.J.,
Metastasis of esophageal squamous cell carcinoma to the thyroid gland with widespread nodal involvement: A case report. World Journal of Clinical Cases.
2020;
8
(19)
:
4588-94
.
View Article PubMed Google Scholar -
Moulick
A.,
Guha
P.,
Das
A.,
Das
A.K.,
Squamous cell carcinoma of proximal esophagus with simultaneous metastases to thyroid and sternum: a case report and review of the literature. Tanaffos.
2012;
11
(1)
:
67-70
.
PubMed Google Scholar -
Milano
A.F.,
Thyroid Cancer: 20-Year Comparative Mortality and Survival Analysis of Six Thyroid Cancer Histologic Subtypes by Age, Sex, Race, Stage, Cohort Entry Time-Period and Disease Duration (SEER\astStat 8.3.2) A Systematic Review of 145,457 Cases for Diagnosis Years 1993-2013. Journal of Insurance Medicine (New York, N.Y.).
2018;
47
(3)
:
143-58
.
View Article PubMed Google Scholar -
Lechner
M.G.,
Bernardo
A.C.,
Lampe
A.,
Praw
S.S.,
Tam
S.H.,
Angell
T.E.,
Changes in Stage Distribution and Disease-Specific Survival in Differentiated Thyroid Cancer with Transition to American Joint Committee on Cancer. The oncologist.
2021;
26
(2)
:
e251--60
.
View Article Google Scholar -
Numata
Y.,
Abe
T.,
Higaki
E.,
Hosoi
T.,
Fujieda
H.,
Nagao
T.,
Should the Supraclavicular Lymph Nodes be Considered Regional Lymph Nodes in Cervical Esophageal Cancer?. Annals of Surgical Oncology.
2022;
29
(1)
:
616-26
.
View Article PubMed Google Scholar -
Cai
Q.,
Hong
Y.,
Huang
X.,
Chen
T.,
Chen
C.,
Current status and prospects of diagnosis and treatment for esophageal cancer with supraclavicular lymph node metastasis. Frontiers in Oncology.
2024;
14
:
1431507
.
View Article PubMed Google Scholar -
Kebebew
E.,
Treatment for Advanced and Metastatic Thyroid Cancer Refractory to Standard Treatment-We Need to Know the When, What, and Who. JAMA Oncology.
2022;
8
(2)
:
250-1
.
View Article PubMed Google Scholar -
Wang
Y.,
Yang
W.,
Wang
Q.,
Zhou
Y.,
Mechanisms of esophageal cancer metastasis and treatment progress. Frontiers in Immunology.
2023;
14
:
1206504
.
View Article PubMed Google Scholar -
Lakshminarayanan
M.,
Kurian
A.,
A Rare Presentation of Metastasis to the Thyroid Gland. Journal of Clinical and Diagnostic Research : JCDR.
2017;
11
(4)
:
19-20
.
View Article PubMed Google Scholar -
Song
Y.,
Driessens
N.,
Costa
M.,
De Deken
X.,
Detours
V.,
Corvilain
B.,
Roles of hydrogen peroxide in thyroid physiology and disease. The Journal of Clinical Endocrinology and Metabolism.
2007;
92
(10)
:
3764-73
.
View Article PubMed Google Scholar -
Nixon
I.J.,
Coca-Pelaz
A.,
Kaleva
A.I.,
Triantafyllou
A.,
Angelos
P.,
Owen
R.P.,
Metastasis to the Thyroid Gland: A Critical Review. Annals of Surgical Oncology.
2017;
24
(6)
:
1533-9
.
View Article PubMed Google Scholar -
Wang
L.Y.,
Palmer
F.L.,
Nixon
I.J.,
Thomas
D.,
Patel
S.G.,
Shaha
A.R.,
Multi-organ distant metastases confer worse disease-specific survival in differentiated thyroid cancer. Thyroid.
2014;
24
(11)
:
1594-9
.
View Article PubMed Google Scholar -
Hegerova
L.,
Griebeler
M.L.,
Reynolds
J.P.,
Henry
M.R.,
Gharib
H.,
Metastasis to the thyroid gland: report of a large series from the Mayo Clinic. American Journal of Clinical Oncology.
2015;
38
(4)
:
338-42
.
View Article PubMed Google Scholar -
Chung
A.Y.,
Tran
T.B.,
Brumund
K.T.,
Weisman
R.A.,
Bouvet
M.,
Metastases to the thyroid: a review of the literature from the last decade. Thyroid.
2012;
22
(3)
:
258-68
.
View Article PubMed Google Scholar -
Ménégaux
F.,
Chigot
J.P.,
[Thyroid metastases]. Annales de Chirurgie.
2001;
126
(10)
:
981-4
.
PubMed Google Scholar -
Chen
H.,
Nicol
T.L.,
Udelsman
R.,
Clinically significant, isolated metastatic disease to the thyroid gland. World Journal of Surgery.
1999;
23
(2)
:
177-80
.
View Article PubMed Google Scholar -
Sahoo
M.,
Bal
C.S.,
Bhatnagar
D.,
Primary squamous-cell carcinoma of the thyroid gland: new evidence in support of follicular epithelial cell origin. Diagnostic Cytopathology.
2002;
27
(4)
:
227-31
.
View Article PubMed Google Scholar -
Limberg
J.,
Ullmann
T.M.,
Stefanova
D.,
Finnerty
B.M.,
Beninato
T.,
Fahey
T.J.,
Prognostic Characteristics of Primary Squamous Cell Carcinoma of the Thyroid: A National Cancer Database Analysis. World Journal of Surgery.
2020;
44
(2)
:
348-55
.
View Article PubMed Google Scholar -
Bejarano
P.A.,
Nikiforov
Y.E.,
Swenson
E.S.,
Biddinger
P.W.,
Thyroid transcription factor-1, thyroglobulin, cytokeratin 7, and cytokeratin 20 in thyroid neoplasms. Applied Immunohistochemistry & Molecular Morphology.
2000;
8
(3)
:
189-94
.
View Article PubMed Google Scholar -
Pusztaszeri
M.P.,
Bongiovanni
M.,
Faquin
W.C.,
Update on the cytologic and molecular features of medullary thyroid carcinoma. Advances in Anatomic Pathology.
2014;
21
(1)
:
26-35
.
View Article PubMed Google Scholar -
Nixon
I.J.,
Whitcher
M.,
Glick
J.,
Palmer
F.L.,
Shaha
A.R.,
Shah
J.P.,
Surgical management of metastases to the thyroid gland. Annals of Surgical Oncology.
2011;
18
(3)
:
800-4
.
View Article PubMed Google Scholar -
Lam
A.K.,
Squamous cell carcinoma of thyroid: a unique type of cancer in World Health Organization Classification. Endocrine-Related Cancer.
2020;
27
(6)
:
177-92
.
View Article PubMed Google Scholar -
Mirallié
E.,
Rigaud
J.,
Mathonnet
M.,
Gibelin
H.,
Regenet
N.,
Hamy
A.,
Management and prognosis of metastases to the thyroid gland. Journal of the American College of Surgeons.
2005;
200
(2)
:
203-7
.
View Article PubMed Google Scholar -
Quan
G.M.,
Pointillart
V.,
Palussière
J.,
Bonichon
F.,
Multidisciplinary treatment and survival of patients with vertebral metastases from thyroid carcinoma. Thyroid.
2012;
22
(2)
:
125-30
.
View Article PubMed Google Scholar -
Park
S.Y.,
Lee
J.,
Jeon
Y.J.,
Cho
J.H.,
Kim
H.K.,
Choi
Y.S.,
Clinical and Pathologic Supraclavicular Lymph Node Metastases in Esophageal Squamous Cell Carcinoma Treated by Esophagectomy with Three-Field Lymph Node Dissection. Annals of Surgical Oncology.
2024;
31
(5)
:
3399-408
.
View Article PubMed Google Scholar -
Baloch
Z.,
Mete
O.,
Asa
S.L.,
Immunohistochemical Biomarkers in Thyroid Pathology. Endocrine Pathology.
2018;
29
(2)
:
91-112
.
View Article PubMed Google Scholar -
Naseri
A.,
Salehi-Pourmehr
H.,
Majidazar
R.,
Seraji
P.,
Rezazadeh-Gavgani
E.,
Zehtabi
M.,
Systematic Review and Meta-analysis of the Most Common Genetic Mutations in Esophageal Squamous Cell Carcinoma. Journal of Gastrointestinal Cancer.
2022;
53
(4)
:
1040-9
.
View Article PubMed Google Scholar -
Zhou
M.,
Yu
S.,
Liu
Y.,
Shu
S.,
Xu
Y.,
Liu
M.,
H3K27me3 Inactivates SFRP1 to Promote Cell Proliferation via Wnt/β-Catenin Signaling Pathway in Esophageal Squamous Cell Carcinoma. Digestive Diseases and Sciences.
2023;
68
(6)
:
2463-73
.
View Article PubMed Google Scholar -
Sharma
U.,
Murmu
M.,
Barwal
T.S.,
Tuli
H.S.,
Jain
M.,
Prakash
H.,
A Pleiotropic Role of Long Non-Coding RNAs in the Modulation of Wnt/β-Catenin and PI3K/Akt/mTOR Signaling Pathways in Esophageal Squamous Cell Carcinoma: Implication in Chemotherapeutic Drug Response. Current Oncology (Toronto, Ont.).
2022;
29
(4)
:
2326-49
.
View Article PubMed Google Scholar -
Li
J.,
Qi
Z.,
Hu
Y.P.,
Wang
Y.X.,
Possible biomarkers for predicting lymph node metastasis of esophageal squamous cell carcinoma: a review. The Journal of International Medical Research.
2019;
47
(2)
:
544-56
.
View Article PubMed Google Scholar -
Haugen
B.R.,
Sherman
S.I.,
Evolving approaches to patients with advanced differentiated thyroid cancer. Endocrine Reviews.
2013;
34
(3)
:
439-55
.
View Article PubMed Google Scholar -
Tsuji
T.,
Matsuda
S.,
Sato
Y.,
Tanaka
K.,
Sasaki
K.,
Watanabe
M.,
Safety and Efficacy of Conversion Therapy After Systemic Chemotherapy in Advanced Esophageal Cancer with Distant Metastases: A Multicenter Retrospective Observational Study. Annals of Surgical Oncology.
2025;
32
:
274-283
.
View Article PubMed Google Scholar -
Wheless
M.C.,
Comer
M.,
Gibson
M.K.,
Evolving Treatment Landscape for Advanced Esophageal and Gastroesophageal Junction Adenocarcinoma. Current Oncology Reports.
2024;
26
(11)
:
1469-88
.
View Article PubMed Google Scholar -
Xin
Z.,
Liu
Q.,
Ai
D.,
Chen
K.,
Mariamidze
E.,
Sumon
M.A.,
Radiotherapy for Advanced Esophageal Cancer: from Palliation to Curation. Current Treatment Options in Oncology.
2023;
24
(11)
:
1568-79
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 11 No 12 (2024)
Page No.: 6971-6977
Published on: 2024-12-31
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 1275 times
- PDF downloaded - 408 times
- XML downloaded - 59 times
 Biomedpress
Biomedpress






