Primary thyroid lymphoma diagnosed by function-preserving lobectomy: a case report
- Department of Oncology, Thai Nguyen University of Medicine and Pharmacy, Thai Nguyen 250000, Viet Nam
- Center for Oncology, Thai Nguyen National Hospital, Thai Nguyen 250000, Viet Nam
- Department of Pathology, Thai Nguyen University of Medicine and Pharmacy, Thai Nguyen 250000, Viet Nam
Abstract
Introduction: Extranodal non-Hodgkin lymphoma of the thyroid, also referred to as primary thyroid lymphoma (PTL), is a rare subtype of non-Hodgkin lymphoma. Clinically, PTL typically manifests as a rapidly enlarging neck mass that may precipitate compressive symptoms. Because of its rarity and non-specific clinical presentation, PTL is often misdiagnosed pre-operatively. In addition to core-needle biopsy, a function-preserving lobectomy with intra-operative frozen-section examination may be appropriate in selected cases. Case description: We describe a 52-year-old Vietnamese woman who presented with a rapidly enlarging, painful and locally inflamed neck mass. Computed tomography revealed multifocal lesions, the largest located in the left thyroid lobe, and suggested chronic thyroiditis. After five days of intravenous antibiotics and corticosteroids, the patient underwent a function-preserving left lobectomy. Definitive histopathology and immunohistochemistry established the diagnosis of PTL. Post-operative 18F-FDG PET/CT was used for staging and the disease was classified as stage IIE non-Hodgkin lymphoma. Conclusion: This case highlights that definitive diagnosis of PTL may be achieved only after lobectomy and underscores the value of a function-preserving approach. Although intra-operative frozen-section analysis failed to detect the lymphoma, it assisted in guiding the extent of resection.
INTRODUCTION
Lymphoma is a malignant neoplasm originating from lymphoid tissues. Although it typically arises in lymph nodes, it can rarely develop from intrathyroidal lymphocytes, a condition referred to as primary thyroid lymphoma (PTL). Primary thyroid lymphoma accounts for approximately 5 % of all thyroid malignancies and fewer than 3 % of extranodal non-Hodgkin lymphomas 1,2. PTL is strongly associated with Hashimoto thyroiditis 3. Clinically, PTL usually presents as a rapidly enlarging neck mass that produces compressive symptoms. The diagnosis is commonly suggested by fine-needle aspiration biopsy (FNAB), particularly in large tumours; however, the limited tissue obtained often renders histopathological evaluation inconclusive for definitive lymphoma confirmation 4. Chemotherapy remains the cornerstone of PTL treatment, yet surgery retains both diagnostic and therapeutic value. Advances in surgical techniques and instrumentation have simplified thyroidectomy for bulky lesions, leading to an increased postoperative identification of rare entities such as PTL. Nevertheless, because of the tumour’s rarity, the optimal role of surgical biopsy remains controversial. Intra-operative assessment by the surgeon, combined with frozen-section analysis, can guide the extent of resection—incisional biopsy, lobectomy, or total thyroidectomy. We describe a Vietnamese woman with PTL who underwent a function-preserving lobectomy for definitive diagnosis. This case underscores the importance of intra-operative evaluation and frozen biopsy in selecting an appropriate surgical strategy and highlights the difficulties inherent in managing large, atypical thyroid malignancies.
CASE PRESENTATION
A 52-year-old woman was admitted to the Oncology Center of Thai Nguyen National Hospital (Vietnam) with a rapidly enlarging, painful mass in the left side of the neck. Approximately twenty days earlier, the patient had noticed a non-tender lump in the same region that produced mild dysphagia. Until the current admission, however, she had not sought medical attention and instead applied poultices prepared by a local traditional healer. After the third application, the symptoms worsened dramatically: the mass grew rapidly, causing severe pain, pronounced dysphagia, and odynophagia, and the overlying skin became erythematous. During the two days preceding hospitalisation, she experienced persistent fever with a maximum temperature of 39.7 °C.
On physical examination, findings were compatible with acute thyroiditis predominantly affecting the left lobe, characterised by localised erythema, warmth, swelling, and marked tenderness. The patient also complained of fatigue secondary to severe dysphagia, odynophagia, and high-grade fever (39.5 °C). No enlarged cervical lymph nodes were palpable, although the assessment was limited by pain.
Laboratory evaluation revealed a red-blood-cell count of 5.71 × 10¹²/L, haemoglobin 14.6 g/dL, platelet count 327 × 10⁹/L, and white-blood-cell count 9.9 × 10⁹/L with neutrophils 59 %. Serum electrolytes and liver enzymes were within normal limits (Na⁺ 139 mmol/L; K⁺ 3.64 mmol/L; Cl⁻ 100.2 mmol/L; AST 20.5 U/L; ALT 20.3 U/L). Thyroid function tests showed TSH 2.15 mIU/mL, T₃ 160.3 ng/dL, free T₄ 1.4 ng/dL; thyroid-specific antibodies were elevated (TSH-receptor antibodies 2.75 IU/L; anti-thyroid peroxidase > 600 IU/mL; anti-thyroglobulin 82.86 U/mL). Calcitonin was 0.51 pmol/L and thyroglobulin 1146 ng/mL. Thyroid ultrasonography demonstrated a 38 × 16 mm poorly defined hypoechoic lesion occupying the left lobe (Figure 1A). Contrast-enhanced neck CT identified two intrathyroidal lesions with well-defined margins and poor enhancement (Figure 1B-C). The imaging appearance was suggestive of chronic thyroiditis consistent with Hashimoto thyroiditis.
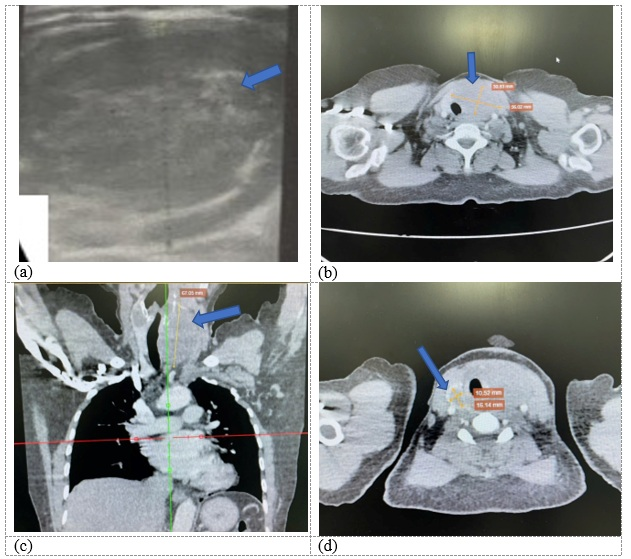
Pre-operative imaging.A) Thyroid ultrasound (transverse view) shows a poorly defined, hypoechoic mass (38 x 16 mm) in the left lobe. B-D) Contrast-enhanced computed tomography (CT) scans of the neck. B, C) A large, well-defined nodule (55 x 38 mm) in the left thyroid lobe with poor contrast enhancement, causing mild compression and displacement of the trachea and esophagus. D) A smaller nodule (14 x 17 mm) in the right thyroid lobe.
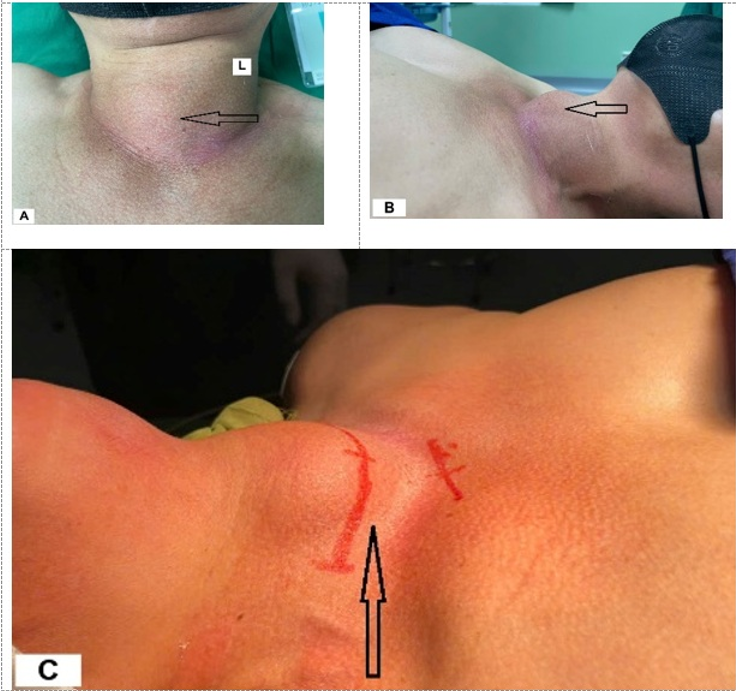
The provisional diagnosis was acute thyroiditis with severe local symptoms. Empirical therapy comprised intravenous cephalothin 1 g every 8 h, methylprednisolone 40 mg/day, paracetamol 2 g/day, and supportive care. After five days, the patient became afebrile and pain-free, dysphagia resolved, and the neck mass decreased in size, although mild erythema persisted (Figure 2A-C).
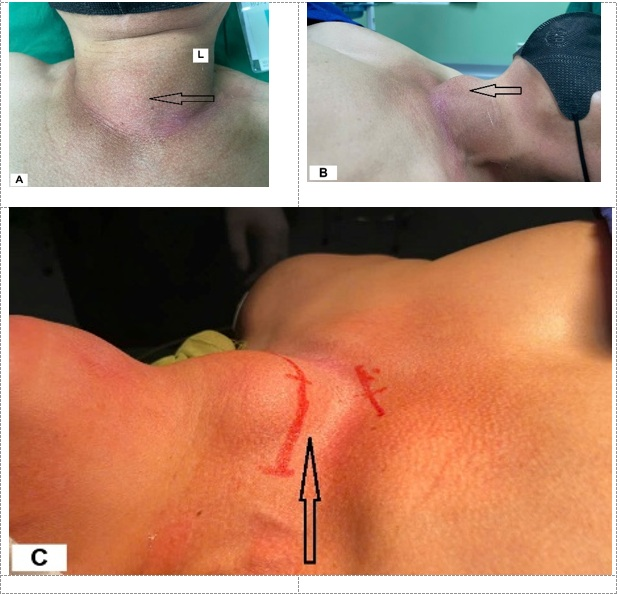
Clinical presentation before treatment. Photographs showing the rapidly enlarging neck mass at admission. A) Superior view demonstrating the tumor predominantly in the left lobe, extending across the midline, with overlying skin erythema. B) Ipsilateral (left) view of the mass. C) Contour of the mass viewed from the contralateral (right) side.
The patient subsequently underwent conventional thyroid surgery. Intra-operatively, the thyroid gland was firmly adherent to the strap muscles, suggesting extrathyroidal extension. A function-preserving left lobectomy was performed, sparing the parathyroid glands and the recurrent laryngeal nerve. The trachea and oesophagus were adherent to the tumour, and a small macroscopic residual mass was intentionally left in situ (Figure 3A-C). Frozen-section analysis indicated lymphoma, and the procedure was terminated, because systemic therapy is the cornerstone of lymphoma management and compressive symptoms were absent.

Intra-operative findings.A) The exposed thyroid tumor (black arrow) appearing whitish, opaque, and friable. Tumor infiltration into the strap muscles is indicated (green arrow). B) The tumor demonstrates extrathyroidal extension, adhering to and infiltrating adjacent tissues. C) View after function-preserving left lobectomy. A small, macroscopic residual tumor was intentionally left behind (black arrow) adjacent to the trachea (green arrow) to preserve critical structures.
Final histopathology revealed non-Hodgkin lymphoma, and immunohistochemistry confirmed diffuse large B-cell lymphoma: CD20 (+), Ki-67 90 %, CD3 (–), CD5 (–), BCL6 (–), MUM1 (–), CD30 (–) (Figure 4).
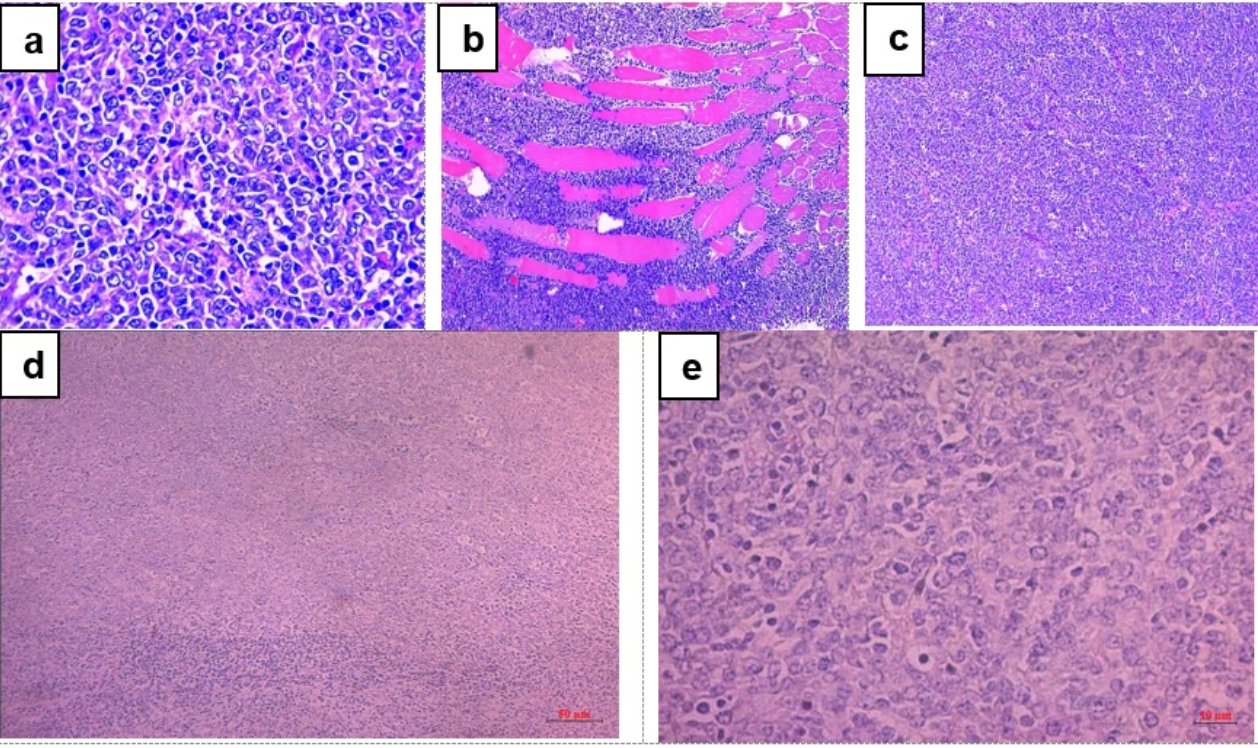
Histopathological analysis (Hematoxylin and Eosin stain). Microscopic examination reveals diffuse infiltration of the thyroid tissue by malignant lymphoblasts. The cells are characterized by large nuclei and numerous abnormal mitotic figures. (a-c: Magnification, ×10; d: Magnification, ×100; e: Magnification, ×400).
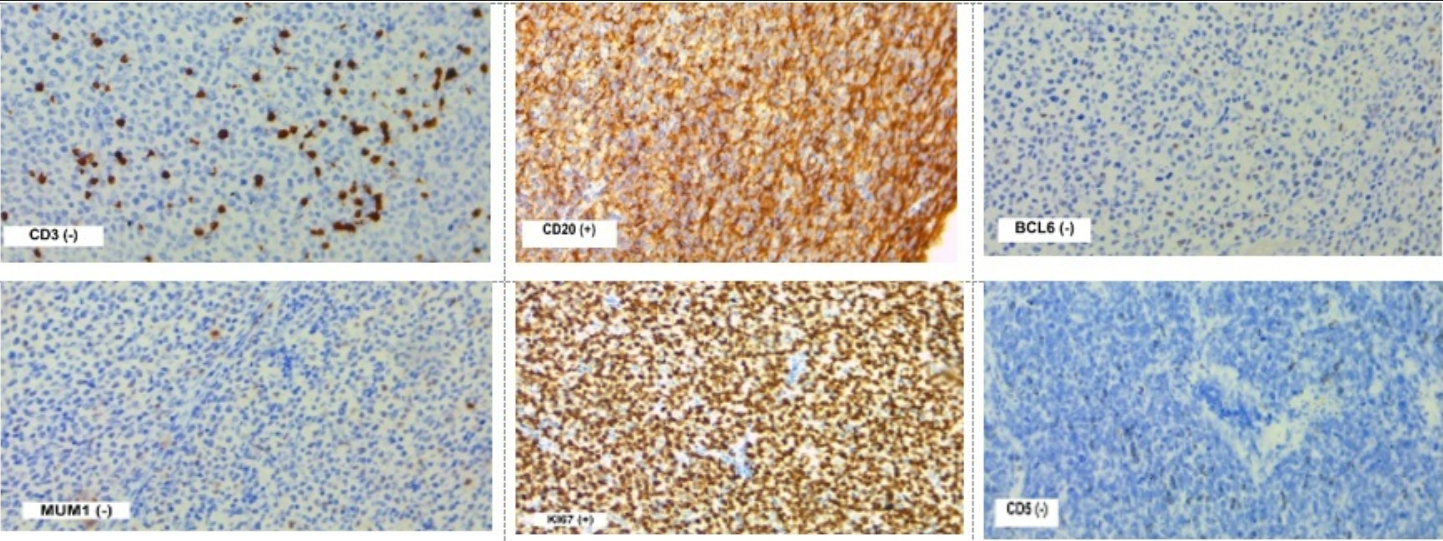
Immunohistochemistry (IHC) profile. IHC staining confirms the diagnosis of diffuse large B-cell lymphoma. The tumor cells are positive for CD20 (a B-cell marker) and show a high proliferation index (Ki-67, 90%). They are negative for the T-cell markers CD3 and CD5, as well as for BCL6, MUM1, and CD30.
The postoperative course was uneventful, and the patient was discharged on day 7. Positron-emission tomography/CT performed before chemotherapy demonstrated stage IIE disease (Figure 6). Seven months after the function-preserving lobectomy, she had completed several cycles of R-CHOP, her thyroid function remained normal (TSH 1.63 mIU/mL; T₃ 159.9 ng/dL; free T₄ 1.2 ng/dL), her voice was normal, and there were no clinical or biochemical signs of hypocalcaemia (total serum calcium 2.49 mmol/L).
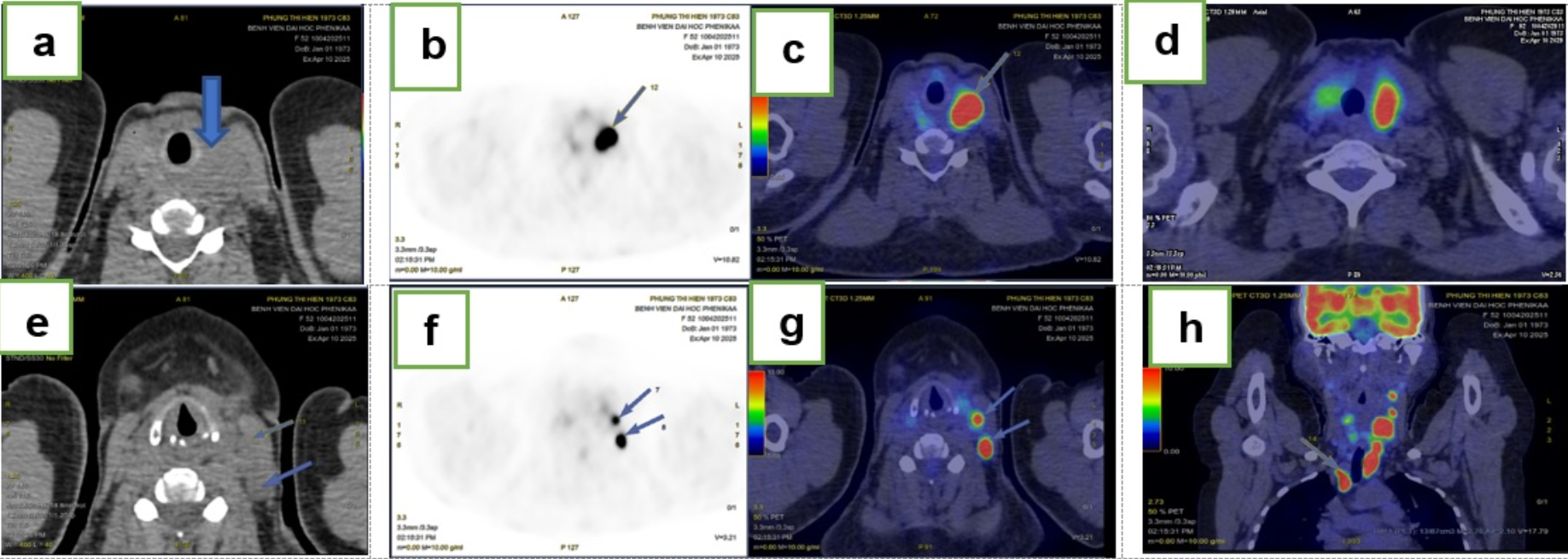
Post-operative staging with ¹⁸F-FDG PET/CT.a-d) Axial, sagittal, and coronal PET/CT fusion images showing multiple foci of intense fluorodeoxyglucose (FDG) uptake in the residual right thyroid lobe (SUVmax: 13.6), indicating extranodal involvement. e-h) Images demonstrating pathological FDG uptake in several cervical (levels II, III, Vb left; bilateral level IV) and mediastinal (bilateral level II) lymph nodes (SUVmax: 24.8), confirming nodal involvement. The findings are consistent with stage IIE disease.
DISCUSSION
Extranodal non-Hodgkin lymphoma of the thyroid, also termed primary thyroid lymphoma (PTL), is a rare malignancy, with few cases reported in the literature (
Reported Cases of Thyroid Lymphoma: Clinical Characteristics, Diagnosis, and Treatment
| Citation | Sex/age | Initial diagnostic test | Diagnosed method | Type of cancer | Stage* | Treatment |
|---|---|---|---|---|---|---|
| Vigliar E et al. (2013). | M/66 and F/68 | Ultrasound | Fine needle cytology, immunocytochemistry | Small B-cell and DLBCL | N/A | CTx based on CHOP and RT |
| Tatari M et al. (2017). | M/65 | Fast-growing neck mass | Total thyroidectomy, IHC | Scleronodular Hodgkin’s lymphoma | IB | N/A |
| Alyami H et al. (2018) | F/66 | Huge neck mass | Tissue biopsy, IHC | DLBCL | N/A | R-CHOP |
| Peixoto R et al. (2012). | F/59 | A rapidly enlarging mass of the anterior compartment of the neck | Total thyroidectomy, IHC | DLBCL | IIE | R-CHOP |
| Tbini M et al. (2024). | M/56 | A neck mass and dysphonia. | Core needle biopsy, IHC | DLBCL | IE | R-CHOP |
| Xatzipsalti M et al. (2023). | F/12 | A right-sided painless progressive swelling of the neck | Ultrasound-guided core needle biopsy, IJC | DLBCL | IIE | CT |
| Hoshino C et al. (2012). | M/73 | Progressive dyspnea with rapid enlargement of the thyroid gland | An incisional biopsy, IHC | DLBCL with germinal centre B-cell subtype. | IIE | R-CHOP and RT |
We describe a 52-year-old Vietnamese woman with PTL. Notably, she had previously undergone a function-preserving left lobectomy. Initially, total thyroidectomy was planned because of multiple nodules; however, on the basis of the frozen-section examination, only a lobectomy was performed. The postoperative course was uneventful, and thyroid function remained normal.
Noble et al. analysed 3,466 patients with PTL between 2004 and 2015; their results showed that lobectomy or thyroidectomy was associated with improved survival compared with non-surgical management 12. In most reported cases, rapid thyroid enlargement is the presenting symptom, and anaplastic thyroid carcinoma must be considered in the differential diagnosis. In the present case, the gland enlarged rapidly and was inflamed, mimicking acute thyroiditis; symptoms diminished markedly after antibiotics and corticosteroids. Pre-operative studies suggested PTL (elevated anti-TPO titre and cytology). The ATA guideline recommends fine-needle aspiration or core-needle biopsy of the thyroid and/or regional lymph nodes for PTL diagnosis. Because of the painful, protruding mass, open surgery was indicated both for diagnosis and symptom relief. As shown in the literature, biopsy techniques vary (
Raquel et al. confirmed the diagnostic value and safety of lobectomy or total thyroidectomy for PTL, although surgery is not the standard treatment 13. Park et al. highlighted the role of surgery in obtaining a definitive diagnosis when cytology is indeterminate and in patients with rapidly enlarging masses 14. Sanchez et al. reported that core-needle biopsy is the preferred diagnostic modality; nevertheless, thyroidectomy was commonly performed in incidentally discovered cases. Among 54 patients, thyroidectomy was undertaken in 22, with lower mortality than in the non-surgical cohort (2/22 vs 8/32, p = 0.172) 15. Beyond diagnosis, thyroidectomy can debulk the tumour, potentially enhancing the efficacy of systemic therapy or radiotherapy and relieving compressive symptoms; however, compared with core-needle biopsy, it carries a risk of tumour spillage and may delay systemic therapy. Wu described a 53-year-old man who underwent right thyroidectomy for tracheal compression; he subsequently developed postoperative dyspnoea owing to rapid regrowth of upper-airway lymphoma 16. Although no postoperative dyspnoea occurred in the present case, vigilance for complications related to tumour spillage is warranted.
In this case, the patient was diagnosed with diffuse large B-cell lymphoma (DLBCL) on the basis of histopathological and immunohistochemical analyses. She subsequently underwent 18F-FDG positron emission tomography/computed tomography (PET/CT) to stage the disease 17. Following surgical recovery, the patient was treated with the rituximab-cyclophosphamide, doxorubicin, vincristine and prednisone (R-CHOP) regimen. After four cycles of R-CHOP, she developed grade 3 leukopenia and pronounced fatigue. She then received involved-site radiotherapy (ISRT) to the cervical region to a cumulative dose of 36 Gy. Post-treatment restaging demonstrated a partial response.
Yoshida et al. reported that the diagnosis-to-treatment interval (DTI)—defined as the time from pathological confirmation to treatment initiation—impacts survival in DLBCL. At 2-year follow-up, patients with a short DTI (≤ 22 days) demonstrated significantly poorer overall survival (62.7 % vs 86.4 %) and progression-free survival (55.1 % vs 75.9 %) compared with those who had a longer DTI (> 22 days) 18. It is evident that patients with primary thyroid lymphoma (PTL) diagnosed by core-needle biopsy (CNB) experience faster recovery than those undergoing diagnostic thyroidectomy. In the present patient, who experienced no postoperative complications, the DTI was 21 days. Patients at high risk for severe complications are not suitable candidates for thyroidectomy.
This case underscores several key clinical considerations. First, a rapidly enlarging thyroid gland in a patient with Hashimoto’s thyroiditis should raise suspicion for PTL. Second, intraoperative frozen-section analysis is crucial for determining the extent of surgery (lobectomy versus thyroidectomy), particularly in patients with bilateral multifocal lesions. Third, function-preserving thyroidectomy may be appropriate when surgical diagnosis of PTL is required. Such surgery aims to obtain adequate tissue while rigorously preserving the parathyroid glands, recurrent laryngeal nerves, adjacent structures (oesophagus, trachea, etc.), and residual thyroid function.
CONCLUSION
Pre-operative diagnosis of PTL remains challenging. PTL should therefore be considered in the differential diagnosis of patients who present with a rapidly enlarging thyroid mass, particularly those with underlying autoimmune thyroiditis. Although intra-operative frozen section analysis may not definitively identify this rare entity, it can still provide valuable guidance in determining the appropriate extent of surgery. For definitive diagnosis, a function-preserving lobectomy represents an effective and judicious surgical option in properly selected patients, permitting histopathological confirmation while minimising procedural complications.
Abbreviations
18F-FDG PET/CT: 18F-fluorodeoxyglucose positron emission tomography/computed tomography; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; ATA: American Thyroid Association; BCL6: B-cell lymphoma 6 protein; CD3: Cluster of Differentiation 3; CD5: Cluster of Differentiation 5; CD20: Cluster of Differentiation 20; CD30: Cluster of Differentiation 30; CNB: Core-needle biopsy; CT: Computed tomography; DLBCL: Diffuse large B-cell lymphoma; DTI: Diagnosis-to-treatment interval; FNAB: Fine-needle aspiration biopsy; ISRT: Involved-site radiotherapy; Ki-67: Marker of proliferation Ki-67; MUM1: Multiple myeloma oncogene 1; PTL: Primary thyroid lymphoma; R-CHOP: Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; T₃: Triiodothyronine; T₄: Thyroxine; TSH: Thyroid-stimulating hormone.
Acknowledgments
None.
Author’s contributions
All authors had been actively involved in the reported case and took full responsibility for the content of this article. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The Hospital’s Ethics Committee waived the need for ethical approval for this case report.
Consent for publication
Written informed consent was obtained from the patient’s mother for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Declaration of generative AI and AI-assisted technologies in the writing process
The authors declare that they have not used generative AI (a type of artificial intelligence technology that can produce various types of content including text, imagery, audio and synthetic data. Examples include ChatGPT, NovelAI, Jasper AI, Rytr AI, DALL-E, etc) and AI-assisted technologies in the writing process before submission.
Competing interests
The authors declare that they have no competing interests.

