
Pharmacological intervention of various Indian medicinal plants in combating COVID-19 infection
- Department of Microbiology, Patna Women’s College, Patna, 800 001, India
- Department of Zoology, P. C. Vigyan Mahavidyalaya, J. P. University, Chapra, 841 301, India
Abstract
Coronavirus pandemic is progressing rapidly causing an eruption of successive waves around the globe due to its ability to cause recurrent mutations, making the prevention and control measures extremely essential. The success of therapeutic benefits of natural plants and herbs are well known to humans since ancient times. Medicinal plants play an important role in curing human diseases due to the presence of phytochemicals and bioactive compounds. India is known for its heritage of medicinal plants, and Traditional Indian Medicines (TIM) have shown the potential to treat several diseases. The review highlights the detailed information of various Indian medicinal plants and their potential therapeutic role as an antiviral and immunomodulatory therapeutics. Ministry of AYUSH (Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homeopathy) has already issued several health advisory and routinely use of medicinal plants to strengthen the immune system to fight against COVID-19. Various medicinal plants, such as Ocimum sanctum, Withania somnifera, Tinospora cordifolia, Curcuma longa, Zingiber officinalis, Azadirachta indica, Piper nigrum, Nigella sativa, Allium sativum, Glycyrrhiza glabra with their antiviral properties against several viruses including SARS-CoV-2 virus have been discussed in the review, which might be an effective prophylaxis against COVID-19. Special emphasis has been given on the antiviral activities of these plants against SARS-CoV-2, highlighting their efficacy as potential drug candidates.
BACKGROUND
Over the centuries, plants and herbs are used as an important source of medicines1 According to WHO, traditional medicines have always been the major source of treatment in primary healthcare system of communities. Right from the evolution of human civilization, the practice of use of medicinal plants have been documented for the purpose of curing human ailments2. The use of medicinal plants take us 5000 years back, providing the primitive evidence of use of traditional medicines in Indian, Chinese, Egyptian, Roman, Greek and Syrian texts3. The vast knowledge of the medicinal values of plants today is the result of long evolution through trials and error when everything was based on experimentations due to which man learned the healing properties of medicinal plants in barks, seeds, fruiting bodies and other parts of plant4. The use of traditional medicines depend on local availability of natural resources and their indigenous knowledge5. About 80% of the health needs of the world’s population is facilitated by herbal medicine, and that too in rural areas of developing countries6. In majority of the developing countries, herbal medication has sustained its popularity, as modern medications are limited in those regions7. According to the reports of WHO, 80% of the population in Africa depends on traditional medicines for health care.
India has always been a land of plants and possesses a rich history of traditional healing system, especially the use of plants and herbs. India has the rich diversity of medicinal plants and Indian herbs are extensively used for the medicinal properties throughout the world8. Forests of India are the major source of therapeutic medicinal plants, contributing to about 90% of the herbs and medicinal plants, with Gujarat, Haryana, Rajasthan, Andhra Pradesh, Uttrakhand and Tamil Nadu being the leading producers of herbal plants in India8. The ancient literatures of India, such as Rigveda, Charak Samhita, Atharvaveda and Sushruta Samhita, talk about the practices of medicinal plants to treat diseases3. In India, around 17,000-18,000 flowering species are found, among which 6,000-7,000 species are considered to have medicinal values3. Apart from the medicinal uses, herbal plants are the source of livelihood to a large section of population of India9. Around 70% population of rural India depends on medicinal plants as a source of treatment of various diseases10. Indians have been using medicinal plants to cure several diseases, treating the wounds and inflammation. Medicinal plants possess several properties and are known to cure some common prevalent diseases, such as malaria, tuberculosis, diarrhoea, asthma and pneumonia11. During the outbreak of epidemic diseases, such as malaria, cholera, small pox in the colonial era, traditional plants were continued to be used in India for medicinal purposes1. Medicinal plants are used against diseases like diabetes, intestinal disorders, parasitic infections, skin disorders, gastrointestinal disorders, neurological disorders, piles, skeletal diseases, viral infections .12. Infectious diseases across the world are the major causes of mortality and are increasing alarmingly within the last few years13. Viral diseases have become a major health concern throughout the world and the emergence of COVID-19 in late 2019 has resulted in a global pandemic.
The Indian Traditional System of Medicines is one of the ancient medical practice in the world14. There are several medicinal plants native to India, which are used as antiviral and immune stimulant14. Various plants, such as . are known to possess the antiviral and immunomodulatory properties which boost the immune system15, 16, 17. The phytochemicals found in plants and the compounds specific to plants, such as flavonoids, saponins, alkaloids, quercetin, catechins and polysulphates play an important role in the inhibition of viral entry of viruses, which further inhibits their replication, causing damage to their nucleocapsid and genetic material16. Therefore, with the help of traditional practices of Indian medicinal plants, new treatment methods can be developed to combat the effects of COVID-19.
A BRIEF OVERVIEW OF CORONAVIRUS
Coronavirus disease 2019 (COVID-19) originated in Wuhan, Hubei Province, China in late December, 201918. It is a positive, single-stranded virus, appearing in a crown shape when seen under an electron microscope, as it has spike glycoprotein on the envelope19. Coronavirus comes under the broad realm of Riboviria, having a total of 39 species20 (Figure 1).

Classification of Coronavirus.
The virus has the largest genome (26.4-31.7kb) among all the RNA viruses known till date21. It has a 5’-cap structure and 3’poly A tail with 14 open reading frames (ORFs) which encode 27 proteins22. There are four structural proteins of the virion, known as S (Spike), E (Envelope), M (Membrane) and N (Nucleocapsid); the S, E and M proteins together constitute the viral envelope, while the protein N holds the RNA genome23. The viral envelope plays a major role in the assembly and release of virus, promoting viral pathogenesis24.
Symptoms of SARS-CoV-2 includes fever, coughing and shortness of breath, but in severe infection, it can lead to pneumonia, multi-organ failure, severe acute respiratory syndrome and even death25, 26. Clinical reports reveal that the most distinctive comorbidities of SARS-CoV-2 were hypertension and diabetes mellitus27. SARS-CoV-2 binds to the host cells through the ACE 2 receptor (Angiotensin converting enzyme 2), which is facilitated by spike glycoprotein, and the process is set with the help of a protease called TMPRSS228, 29. After further endocytosis followed by uncoating, components of SARS-CoV-2 with the aid of host cell machinery produce new viruses. As a result of stimulation of SARS-CoV-2, the host immune system releases cytokines following inflammation through activation of dendritic cells, NK cells, macrophages, and neutrophils, which can result into sepsis, multiple organ failure, septic shock and even death30. The expression of ACE 2 is high in heart, kidney, blood vessels, lungs and intestine31. Multiplication of viruses induce cellular responses comprising of innate and adaptive immune cells32, 33. Neutrophils produces injury to lungs and adaptive immune cells, mainly the T cells (Cytotoxic CD8 T cells), which not just kill the virus, but also causes injury to lungs34, 35. This triggers the progression of systemic inflammatory response called cytokine surge, in which there is an extensive increase in the number of cytokines (TNF-α, IL1, IL6, IL10 .) which thereby causes inflammation and cell death of Type 1 and Type 2 cells in the alveoli36. This causes the interruption in transportation of oxygen, resulting in apoptosis in alveoli of the lungs and hence causes Acute Respiratory Distress or Syndrome (ARDS)37. Transmission of SARS-CoV-2 virus occurs from human to human through respiratory droplets during coughing and sneezing38.The high affinity of S-protein of SARS-CoV-2 to bind ACE 2 is 10 - 20 fold greater than S protein of SARS-CoV, due to which SARS-CoV-2 spreads rapidly31.
In the race to curb the spread of the novel Coronavirus, several strategies and measures are being implemented from social distancing to drugs and vaccine discoveries. In addition, traditional herbal medicines are also being explored side by side as there is still huge dependence on medicinal plants as complementary medicines39. As we know that SARS-CoV-2 affects weak, immune compromised people, herbal medicines can play a potential role in boosting the immune system and possess antiviral properties which can curb the effects of COVID-19, lowering down the death rates worldwide40.
STATUS OF MEDICINAL PLANTS OF INDIA
Humans depend on nature and its source for survival and sustenance. Plants have been one of the important sources of medicines, and in India, curative properties of plants take us back to the age of the Rigveda (2500 to 1600 B.C.)1. Traditional herbal medicines hold a long history in treating various infectious diseases due to the presence of anti-bacterial, anti-viral, anti-inflammatory and immunomodulatory properties, which make them effective against a wide array of diseases41, 39, 42. India has a rich traditional healing system, and the oldest printed book on Indian Medicinal Plants, enlists the use of the medicinal plants. The most ancient written evidence of usage of medicinal plants for the preparation of medicine has been found from Nagpur on Sumerian clay slab, which dates back to 5000 years ago4. In India, there are more than 1.5 million practitioners who use traditional medicine system for healthcare, and more than 1500 herbal formulations are sold as dietary supplements10, 43. 1000 species of medicinal plants are reported in India, among which 540 species are herbs, 100 are shrubs, 160 climbers, 200 species are trees, orchids are 15 species and ferns and conifers are 2044. 70% of Indian medicinal plants are found in tropical forests of Eastern and Western Ghats, Himalayas, Aravali Vindhya range and Chota Nagpur Plateau45.
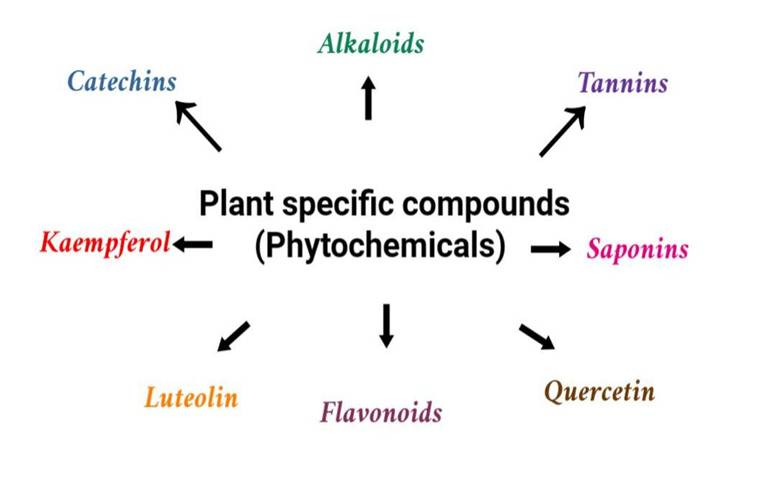
Types of plant specific compounds (Phytochemicals).
Despite the progress of modern medical and pharmaceutical research, the use of medicinal plants are still significant and common, and the Indian Traditional System of Medicines (Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homeopathy (AYUSH)) uses herbs and plants for treatment of various diseases1 (
National Medicinal Plant Board (NMPB), established in India in November 2000 by Government of India, acts as a primary board for coordinating all matters related to medicinal plants, their growth, export, conservation and cultivation. This board is located in Department of AYUSH of Ministry of Health and Family Welfare, Government of India3.
List of some common medicinal plants found in India
|
Local Name |
English Name |
Botanical Name |
Parts used |
Applications |
|---|---|---|---|---|
|
Tulsi |
Holy basil |
|
Leaves |
antiallergic, antidiabetic |
|
Methi |
Fenugreek |
|
Seeds |
constipation, diabetes |
|
Dalchini |
Bark Cinnamon |
|
antibacterial, antiseptic | |
|
Amla |
Indian gooseberry |
|
Fruit |
constipation, antioxidant, fever, diabetes, hyperacidity |
|
Mulethi |
Licorice |
|
Roots |
digestive disorders, ulcers, bronchitis |
|
Pyaj |
Onion |
|
Bulb |
prostate cancer, stomach cancer |
|
Ghritkumari |
Aloe |
|
Leaves |
laxative, wound healing, skin burns, ulcers |
|
Ashwagandha |
Indian ginseng |
|
Roots, leaves |
restorative tonic, stress, nerves disorders, aphrodisiac |
|
Elaichi |
Lesser Cardamom |
|
Pod and seeds |
nausea, vomiting, dry cough |
|
Babool |
Gum arabic tree |
|
Bark, root, gum, leaves, pods, seeds |
oral care, bleeding gums, wounds |
|
Lehsun |
Garlic |
|
Bulb |
ringworm, dysentery, wounds, heart diseases |
|
Neem |
Margosa tree |
|
Root, bark, flower |
cough, diabetes, skin diseases, arthritis, bronchitis |
|
Chirayata |
Bitter stick, East Indian Balmony, |
|
Whole plant |
fever and jaundice |
|
Harad |
Chebulic Myrobalan |
|
Fruits, roots, bark |
digestive disorders, eye and skin diseases |
|
Doob |
Bermuda grass |
|
Leaves |
jaundice, antidiarrheal |
|
Adrak |
Ginger |
|
Rhizome |
antioxidant and anti-arthritic |
|
Giloe/Guduchi |
Heart-leaved moonseed |
|
Stem |
fever, urinary diseases, dyspepsia |
|
Sadabahar |
Madagascar Periwinkle |
|
Whole plant |
leukaemia, hypertension, antispasmodic |
|
Sarpgandha |
Indian snakeroot |
|
Root |
hypertension, insomnia |
|
Jyotishmati |
Staff tree |
|
Seeds |
gout, neurological disorders, rheumatism |
|
Laung |
Clove |
|
Dried flower buds, leaves, and stems |
analgesic, antioxidant, antitumor, antiviral, antifungal, anti- inflammatory and antibacterial activity |
|
Haldi |
Turmeric |
|
Rhizome |
anti-inflammatory, hematuria, hemorrhage, flatulence, jaundice, menstrual difficulties |
|
Guggul |
Indian bdellium-tree |
|
Bark |
urinary infections, ascites, piles, arthritis, swellings ulcers and in skin diseases |
|
Bhringaraj |
False daisy |
|
Whole plant |
hepatotoxicity |
|
Paan |
Betel |
|
Leaf |
anti-inflammatory, anti-apoptotic, anti-oxidant, anticancer and antibacterial activity |
|
Peepal |
Sacred fig |
|
Bark, leaves, fruit, seeds, latex |
constipation, gynecological diseases and skin diseases |
|
Datura |
Thorn apples |
|
Leaves and fruits |
asthma, cardiac pains |
List of some common medicinal plants of India having antiviral properties
|
Plants (Scientific Name) |
English name |
Family |
Effective against virus |
Reference |
|---|---|---|---|---|
|
|
Indian ginseng |
Solanaceae |
HSV-1 |
|
|
|
Roselle |
Malvaceae |
Measles |
|
|
|
Liquorice |
Fabaceae |
Japanese encephalitis, Polio |
|
|
|
Indian gooseberry |
Euphorbiaceae |
Polio |
|
|
|
Holy Basil |
Lamiaceae |
Vaccinia |
|
|
|
Lesser galangal |
Zingiberaceae |
H1N1 |
|
|
|
Ginger |
Zingiberaceae |
Hepatitis C |
|
|
|
Florist’s daisy |
Asteraceae |
HIV-1 |
|
|
|
Cape jasmine |
Rubiaceae |
Influenza |
|
|
|
Chinese cassia, Chinese cinnamon |
Lauraceae |
HIV-1, HIV-2 |
|
|
|
Garlic |
Alliaceae |
SARS |
|
|
|
Indian wild pepper |
Lamiaceae |
SARS-CoV |
|
|
|
Gray mangrove |
Avecennaceae |
Fowl pox |
|
|
|
Pomegranate |
Puniaceae |
Influenza |
|
|
|
Black cumin |
Ranunculaceae |
Newcastle |
|
|
|
Great millet |
Poaceae |
HSV-1 |
|
ANTIVIRAL ACTIVITY OF INDIAN MEDICINAL PLANTS
Earth contains around 10 viruses, and they are ubiquitous even in the marine environment, as nearly 5000 viral genotypes are present in every 200 L of water62, 63. Viral diseases are increasing throughout the world and are a matter of great concern64. They enter the body and redirect body’s metabolism to produce multiple copies of their genome and proteins65. Plants contain a variety of bioactive constituents, such as alkaloids, phenolic compounds, saponins, flavonoids, lignans and other bioactive components which make them a suitable treatment option against viral infections66, 67, 64. Studies reveal that compounds, such as andrographolide, glycyrrhizic acid, curcumin as well as extracts of have antiviral activities68. Antiviral activities of plants like , , are well known65. Antiviral activities of 38 Indian plants have been reported in 32 papers to be effective against human immunodeficiency virus (HIV)68. In another study by Mehrotra .69 neutralizing activity of has been reported against hepatitis virus. Ahmed and Verma70 studied the genus (Euphorbiacae) and worked on plants namely which showed pharmacological and phytochemical properties of the genus exhibiting diverse biological activities such as antihepatotoxicity, anti-HIV, anti-carcinogenic and anti-inflammatory properties. Indian plants, such as (Family-Fabaceae), (Family-Avecennaceae), (Family-Vitaceae), (Family-Convolvulaceae), (Family-Aristolocheaceae), (Family-Fabaceae), (Family-Mimosaceaeare), (Family-Zygophyllaceae) and (Family-Capparidaceae) are found to possess antiviral properties against pox viruses 59 (
(Family- Rhizophoraceae) was assessed for its antiviral activities against Human immunodeficiency virus (HIV) cell culture system and the polysaccharide extracted from the bark of was found to be inhibiting the viral cycle as it protected MT-4 cells from HIV induced cytopathogenicity and inhibited expression of HIV antigens71. Fiore 72 reported antiviral activity of spp. (Licorice) against HIV-1, SARS related Coronavirus, hepatitis B virus, vaccinia virus and vesicular stomatitis virus, as it reduces transportation of the virus to the membrane and sialyation of surface antigen of hepatitis B virus inhibits fusion of the viral membrane of HIV-1 with the cell by reducing membrane fluidity. It also induces interferon gamma in T cells and inhibition of phosphorylating enzymes in the infection by vesicular stomatitis virus.
commonly known as neem (Family- Meliaceae), native to Indian subcontinent, is another promising plant having active component azadirachtin and other constituents such as nimbidol, sodium nimbinate, gedunin, salannin, quercetin, nimbolinin, nimbin and nimbidin, and holds a long history of use in traditional medicines throughout the world73. Extracts of neem have shown antiviral activity on viruses such as vaccinia, Buffalo pox, chikunguniya, herpes, measles 68.
Central Drug Research Institute, Lucknow (CDRI) screened top 11 families for their pharmacological activities, and the rank of 11 families on the basis of their antiviral activities were found to be in this order: Euphorbiaceae > Fabaceae > Asteraceae > Fagaceae > Myrtaceae > Rubiaceae > Rosaceae > Caesalpineaceae > Lamiaceae > Lauraceae > Anacardiaceae68.
INDIAN MEDICINAL PLANTS EFFECTIVE AGAINST COVID-19
Medicinal plants are known to have antiviral properties and several health benefits and their bioactive constituents may provide help in designing novel alternative and supplementary treatment for COVID-1974. Due to less cost, easier availability and no side effects, majority of the Indian population rely upon herbal medicines40. Several plants of Indian origin have been quoted to possess antiviral activity against SARS-COV-275. Certain medicinal plants have been recommended by India for prevention and prophylaxis of coronavirus, such as , , , and 76. The medicinal drugs for coronavirus can be derived from turmeric, ginger, tulsi, fenugreek, cloves, cinnamon and fennel seeds77.
As per the study conducted by Srivastava.78, 18 different species of Indian herbal plants were assessed in the pursuit of potent COVID-19 inhibitors through and the inhibition potentials of the plant were in order as follows: harsingar > aloevera > giloy > turmeric > neem > ashwagandha > redonion > tulsi > cannabis > black pepper, on the basis of lipophilicity, aqueous solubility and binding affinity. Molecular docking study against Mpro and ACE 2 showed that phytochemicals present in plants, such as have better binding energy with Mpro and ACE-2 as studied by Joshi .79.
In another research done by Maurya and Sharma80, phytochemicals and bioactive compounds present in tulsi, haldi, giloy, ginger, cloves, lemon, ashwagandha and ginger were assessed using molecular docking approach against SARS-CoV-2. The compounds in herbs were docked with viral capsid spike and protease to study their antiviral activities, and the phytochemicals were found potentially efficient in inhibiting different stages of SARS-CoV-2 infection and its target proteins. As studied by Shree 81, the compounds obtained from , and could bind to SARS-CoV-2 Mpro and was found to decrease the viral transcription and replication serving as a potential inhibitors .
Ocimum sanctum
Family: Labiatae; Lamiaceae
English Name: Holy Basil, Sacred Basil
Ayurvedic Name: Tulasi, Surasaa, Bhuutaghni, Sulabhaa, Manjarikaa, Suravalli, Bahumanjari, Devadundubhi, Apet-raakshasi, Shuu-laghni, Graamya, Sulabhaa
Unani: Tulasi
Siddha: Tulasi, Nalla-Tulasi
Habitat: Grown throughout Indian houses, gardens and temples.
In Ayurveda, Tulsi is known as ‘Elixir of Life’ due to its curative properties and several heath ailments such as bronchitis, asthma, gastric and hepatic disorders, microbial infections, rheumatism 40. is used as a nervine tonic and adaptogen, and is known for its stress releasing properties and improving health conditions during cancer82, 83. Compounds including phenolics, flavonoids, phenylpropanoids, essential oil, fixed oil, terpenoids, coumarins and fatty acid derievatives are found in tulsi. Extracts of methanol and dichloromethane from exhibit an anti-HSV activity as reported by Caamal-Herrera .84, Tang .85 and Ghoke .86 reported the antiviral activities of methanol extract (terpenoids and polyphenols) against DENV1 and H9N2. Tulsi contains Tulsinol (A, B, C, D, E, F, G) and dihydrodieugenol-B which inhibits COVID-19 main protease and papain like protease, and also possess ACE 2 blocking properties with immune-modulatory feature87, 88. According to the research done by Mohapatra .89 the ethanolic extract of aerial parts of Holy Basil contain flavonoids and polyphenolic acids especially luteolin-7-O-glucuronide and chlorogenic acid may bind covalently to the active residue Cys145 of main protease of SARS-CoV-2 and inhibit the viral enzyme irreversibly when screened .
Withania somnifera
Family: Solanaceae
English name: Winter Cherry, Indian ginseng, Poison gooseberry
Ayurvedic name: Ashwagandhaa, Ashwakanda, Gandharva-gandhaa, Varadaa, Balyaa, Turaga, Turagagandhaa, Haya-gandhaa, Turangagandhaa, Vaajigandhaa, Gokarnaa, Vrishaa, Varaahakarni, Varadaa, Balyaa, Vaajikari
Unani: Asgandh
Siddha: Amukkuramkizhangu
Habitat: Throughout the drier and semitropic parts of India
Ashwagandha means “the smell and strength of a horse”, referring to its aphrodisiac properties. Roots of is used as an anti-inflammatory medicine for swellings, tumours and as a sedative; root contains alkaloids such as withanine, psuedo-withanine, somnine, somniferinine and withaferin A90. Withaferin A obtained from Ashwagandha is used to treat common cold, gynaecological disorders and infertility issues77. They are known to enhance nitric oxide synthase activity of macrophages and restore immune homeostasis91. They can reduce interleukin-1, interleukin-6 and tumour necrosis factor92, 93, 94. Antioxidant and immune-modulatory effects of Ashwagandha have been studied over the last two decades, and the studies claim it to be effective in boosting immune response and in inhibiting viral replication95, 96. Grover .97 studied this plant through molecular docking approach, and reported the potential role of withaferin A against HSV by inhibition of DNA Polymerase enzyme. Balkrishna .98 reported that withanone (a compound found in ) docked the binding interface of ACE 2-RBD (Receptor Binding Domain) complex, reduced the electrostatic component of binding free energies of ACE2-RBD complex and destabilized the salt bridges at the interface centre, significantly decreasing their occupancies. As Ashwagandha prevents cytokine storms as well as viral infections, it can be a potential candidate for treatment of SARS-CoV-291. Withanolides, a group of bioactive compound found in are potent immunity boosters; Withanolide _G, Withanolide_I and Withanolide_ M have the highest binding affinity with PLpro, 3CLpro and spike proteins respectively99. It can prove to be effective against SARS-CoV-2 through modulation of host Th-1/Th-2 immunity87.
Tinospora cordifolia
Family: Menispermaceae
English name: Heart leaved moonseed
Ayurvedic name: Guduuchikaa, Guluuchi, Amrita, Amritaa, Amritalataa, Amritavall, Chinnaruuhaa, Chinnodbhavaa, Madhuparni, Vatsaadani, Tantrikaa, Kundalini, Guduuchisattva (starch)
Unani: Gilo, Gulanchaa. Sat-e-Gilo
Siddha: Seenil, Amrida-valli
Habitat: Tropical India and the Andamans
It is considered as the best rasayana due to its strong flexibility, and the herb is known to play an important role in boosting immune system77. methanol extracts possess anti-bacterial properties against and 100. The antiviral properties of against H1N1 and Chikungunya virus have already been documented by researchers101. The immune-modulatory property of is well documented due to presence of compounds magnoflorine, tinocordiside, syringin, 11-hydroxymustakone, N-methyl-2-pyrrolidone, N-formylannonain and cordifolioside100, 102. It is known as the nectar of life103
According to Sagar and Kumar101, the binding efficacy of natural components Berberine, Isocolumbin, Magnoflorine and Tinocordiside isolated from were assessed using tools against four SARS-CoV-2 targets (Receptor binding domain (6M0J), surface glycoprotein (6VSB), RNA dependent RNA polymerase (6M71) and main protease (6Y84)), and all the four compounds showed high binding efficacy against all the four targets, making giloy a potential herb for the management of COVID-19 infection.
Curcuma longa
Family: Zingiberaceae
English name: Turmeric
Ayurvedic name: Priyaka, Haridruma, Kshanda, Gauri, Haridraa Kaanchani, Krimighna, Varavarnini, Yoshitapriyaa, Kshanda, Hattavilaasini, Naktaahvaa, Sharvari
Unani: Zard Chob
Siddha: Manjal
Habitat: Grown all over India, particularly in West Bengal, Tamil Nadu and Maharashtra
Turmeric is a herbaceous, perennial, rhizomatous plant, and is widely used in Ayurveda, Siddha and traditional Chinese medicines104. Curcumin (diferuloylmethane), the natural polyphenolic compound found in makes up the major curcuminoid (77%), while curcumin II and curcumin III make up 17% and 3% respectively105. Curcumin exhibits therapeutic properties, such as antimicrobial, antiviral and anti-inflammatory activities91. The antiviral activity of curcumin is well documented, and evidences suggest that it has inhibitory effects against viruses, such as herpes simplex virus, respiratory syncytial virus, vesicular stomatitis virus, flock house virus and parainfluenza virus type 3106. Curcumin relieves congestion and pain, and improves breathing process in patients with sinusitis107. Turmeric acts as a natural cleanser of the respiratory tract. Curcumin contains anti-thrombotic properties, which aid in cleansing mucous in the lungs, thereby supporting proper oxygen supply to the entire body108.
Das .109 reported that curcumin isolated from turmeric can neutralize the entry of SARS-CoV-2 viral protein. The study used approach, which demonstrated the binding of curcumin to RBD site of viral S protein along with the viral attachment sites of ACE 2 receptor. Curcumin can suppress pulmonary edema and fibrosis-associated pathways associated with COVID-19 infection110. It has several molecular mechanisms and inhibitory effects on toll like receptor, inflammatory cytokines, chemokines and bradykinin111. Diacetylcurcumin isolated from have been found more effective on SARS-CoV-2 (Mpro) compared to Nelfinavir112. Immunity and protective defence against COVID-19 infections boosted in many hospitalized patients in India due to the uptake of curcumin with vitamin C and Zinc113. Therefore, curcumin could be considered as a preventive herb in the inhibition of transmission of COVID-19.
Zingiber officinalis
Family: Zingiberaceae
English name: Ginger
Ayurvedic name: Aardraka, Aadrikaa, Shrngibera, Shrngavera, Katubhadra
Unani: Zanjabeel-e-Ratab, Al-Zanjabeel
Siddha: Allam, Lokottai, Inji
Habitat: Indigenous to Southeast Asia; cultivated mainly in Kerala, West Bengal, Andhra Pradesh, Uttar Pradesh and Maharashtra
Ginger is used as a common traditional medicinal plant having therapeutic properties, such as antibacterial, antioxidant, antiviral, analgesic and antipyretic properties114. The phytocompound 6-gingerol obtained from ginger depicts ginger as a promising candidate for drug discovery against COVID-19, as it proved to have the highest binding affinity with multiple targets of SARS-CoV-2, such as viral protease, RNA binding proteins and viral proteases through DFT (Density Functional Theory) study115. Ginger is known to strengthen body’s defense mechanism by improving the antioxidant property. 6-Shogaol, an important compound obtained from ginger, helps the patient in relieving respiratory issues77. Aqueous extract of fresh ginger showed antiviral activity against human respiratory syncytial virus in human respiratory tract cell lines (Hep-2(human laryngeal carcinoma) and A549 (Adeno carcinomic human alveolar)), reducing the plaque count14. According to Chang .116, ginger stimulates IFN-β secretion which counteracts viral infection. Reduction in total nasal symptom scores (TNSS) in patients suffering from rhinitis allergy was also reported by taking oral alcoholic ginger extract117.
Azadirachta indica
Family: Meliaceae
English name: Neem tree, Margosa tree
Ayurvedic name: Arishtaphala, Pichumarda, Pichumandaka, Tiktaka, Sutiktak, Paaribhadra, Nimbaka, Arishta
Unani: Aazaad-Darakht-e-Hindi
Siddha: Vemmu, Veppu, Veppan, Arulundi
Habitat: local to Burma; found all over India
Neem extract compounds have antiviral, anti-inflammatory, anti-hyperglycaemic, anti-carcinogenic, anti-mutagenic, anti-ulcer and anti-oxidant effects118. The important phytochemicals present in neem are limonoids and terpene119. Antiviral activity of aqueous neem leaf extract is well documented against measles, Chikungunya and vaccinia virus120. Earlier studies have revealed that neem and its phytoconstituents play an important role in scavenging of free radical generation and prevents the pathogenesis of diseases73.
Baildya .121 studied the inhibitory potential of neem extracts on PLpro (papain like protease) of SARS-CoV-2 through molecular docking and molecular dynamics simulation, and it was found that desacetylgedunin (DCG) found in neem showed the highest binding affinity towards PLpro. The bioactive compound found in neem, such as Azadiradione, Epiazadiradione, Nimbione, and Vepnin were assessed by Sharon122 through Autodock 4.2, and Pymol and was found to be potential inhibitor of COVID-19 Mpro (6Y2E, 6LU7, and 2GTB).
Nigella sativa
Family: Ranunculaceae
English name: Black Cumin, Small Fennel
Ayurvedic name: Kaalaajaaji, Kalikaa, Prthvikaa, Sthulajiraka, Sushavi, Upkunchikaa
Unani: Kalonji, Kamaazaruus
Siddha: Karumseeragm
Habitat: Cultivated in Assam, Punjab, Bengal and Bihar
Prophet Muhammad quoted, ‘In the black cumin, there is a cure for every disease except death,’ and the Holy Bible denotes black cumin as a ‘curative black seed’123. The phytoconstituents found in black cumin are terpenes such as dithymoquinone (DTQ), carvone, thymoquinone (TQ), limonine, trans-anethol, and p-cymene, indazole alkaloids like nigellidine and nigellicine, isoquinoline alkaloids including nigellicimine, nigellicimine-N-oxide and α-hederin124. It is known for its curative properties, including jaundice, diabetes, cough, bronchitis, fever, gastrointestinal, conjunctivitis, asthma and rheumatism125.
Studies have shown that TQ has an inhibitory property on SARS-CoV-2 protease, and has shown good antagonism to ACE 2 receptors126. Koshak and Koshak127reported that at least eight studies have demonstrated that compounds of have moderate to high affinity with SARS-CoV-2 enzymes and proteins.
Piper nigrum
Family: Piperaceae
English name: Black Pepper
Ayurvedic name: Maricha, Vellaja, Uushna, Suvrrita
Unani: Filfil Siyaah, Safed
Siddha: Milagu, Milaguver
Habitat: Locally found in the Indo-Malaysian region, cultivated in Western Ghats, Karnataka, Maharashtra, Assam and Kerala
It is known as the ‘King of Spices’. Piperine found in black pepper is widely known for its antitumour, anti-asthmatic, antihypertension and anti-carcinogenic properties128. The alkaloid constituents present in black pepper gives it the characteristic strong smell129. According to Choudhary .130, peperine isolated from black pepper can be effective against proliferation of viral particles, as it can block RNA packaging inside the capsid protein. Researchers from Department of Physics at IIT, Dhanbad conducted a computational study and found that Piperine found in black pepper can inhibit SARS-CoV-2 virus. The phenolic compunds Kadsurenin L and methysticin found in was found inhibiting COVID-19 main protease as studied by Davella .131.
Allium sativum
Family: Liliaceae, Alliaceae
English name: Garlic
Ayurvedic name: Lashuna, Yavaneshta, Ugragandha, Rasona, Mahaushadh, Arishta
Unani: Seer, Lahsun
Siddha: Ullippoondu, Vellaippondu
Habitat: Cultivated all over India
The beneficial properties of garlic are known to humans from ages. The chemical constituents of garlic, which are responsible for its peculiar smell and taste, are mainly sulphur-based, such as S-allyl cysteine, alliin, vinyldithiin, ajoene, diallylpolysulfides, and some non-sulphur, such as saponins, maillard reaction products and flavonoids40. Garlic acts as an immunomodulatory by stimulating WBC, such as NK cells and macrophages132. Garlic induces cytokine secretion and increases CD4 and CD8 cells133. Shojai .134reported that concentration of 0.1 ml of garlic clove extract showed inhibitory effects against SARS-CoV-1 multiplication, possibly due to the blocking capacity of extract towards its structural proteins. Alliin found in showed the highest binding ability, with the target protein of SARS-CoV- 2 (6LU7) when studied by Pandey 135. Bioactives found in garlic and the serine-type protease found in SARS-CoV-2 form hydrogen bonds in the active site regions suppressing the outbreak of COVID-19, and it can act as a preventive measure against COVID-19 infection136.
Glycyrrhiza glabra
Family: Papilionaceae; Fabaceae
English name: Licorice, Liquorice
Ayurvedic name: Yashtimadhu, Madhuyashtyaahvaa, Madhuli, Madhuyashtikaa, Atirasaa, Madhurasaa, Madhuka, Yastikaahva, Yashtyaahva, Yashti, Yashtika, Yashtimadhuka
Unani: Asl-us-soos, Mulethi
Siddha: Athimathuram
Habitat: Native to the Mediterranean regions. Now cultivated in Punjab, Jammu and Kashmir, and South India.
Glycyrrhizic acid, found in the roots of , is the active antiviral compound which possesses antiviral activity against HIV, herpes simplex viruses and human and animal coronavirus137. Zhong .138 documented the viral replication inhibitory property of licorice for various viruses, such as influenza, HIV, H1N1, hepatitis B and C.
Zhang .139 assessed licorice, demonstrating that it contains three orally antiviral natural components which inhibit Mpro, S-proteins, 3C like protease and papain like protease of SARS-CoV-2. Licorice extract inhibits the main protease of SARS-CoV-2, and glycyrrhizin shows a high binding affinity and better ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties compared to other constituents of licorice40. Luo .140 discussed the pharmacological action of glycyrrhizin, as it binds to ACE-2, inhibits accumulation of intracellular reactive oxygen species (ROS), inhibits hyperproduction of airway exudates and induction of endogenous interferons141. van de Sand .142 demonstrated that glycyrrhizin inhibits 3CL protease of SARS-CoV-2. Different concentrations of glycyrrhizin 30 µM and 2000 µM and the complete protease inhibitor GC376 were dissolved with 90 ng Mpro in 30 µL 0.5 M DTT buffer at room temperature for 30 mins, after which the 3CL Protease substrate was added, and the activity of protease was measured after overnight incubation at the wavelength 360 nm/460nm (exc/em). It was found that glycyrrhizin inhibited Mpro activity completely at a concentration of 2000 µM, and at 30 µM concentration, it reduced its activity to 70.3%.
CONCLUSION
India has always been known for its rich biodiversity and extensive varieties of plants, which are found from Himalayas to the marine and desert to the rain forests. The present study revealed the status of medicinal plants and herbs of India and their various therapeutic benefits. Use of herbal medicines is not only safe and cost-effective, but it is also free from side effects. AYUSH system of medication emphasizes on simple natural remedies for the improvement and development of strong immune system.
Efforts should be made to explore and promote the knowledge of healing through such medicinal plants. The proper use of medicinal plants against COVID-19 could safeguard lives of several people reducing the risks of infection, thereby minimizing the rate of mortality.
Abbreviations
3CLpro: 3- Chymotrypsin Like Protease
ACE 2: Angiotensin converting enzyme 2
ADMET: Absorption, Distribution, Metabolism, Excretion, and Toxicity
ARDS: Acute Respiratory Distress or Syndrome
AYUSH: Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homeopathy
DCG: Desacetylgedunin
DFT: Density Functional Theory
DTQ: Dithymoquinone
NMPB: National Medicinal Plant Board
PLpro: Papain Like Protease
RBD: Receptor Binding Domain
ROS: Reactive Oxygen Species
TIM: Traditional Indian Medicines
TMPRSS2: Transmembrane Protease Serine 2
TNSS: Total Nasal Symptom Scores
Acknowledgments
None.
Author’s contributions
All authors equally contributed in this work. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.

