A Pilot Study on Implementing Home Blood Pressure Telemonitoring for Older Adults with Mild Cognitive Impairment in Viet Nam
- University of Health Science, Vietnam National University, Ho Chi Minh City. Address: Linh Trung Ward, Thu Duc City, Ho Chi Minh City, Viet Nam
- University of Medicine and Pharmacy at Ho Chi Minh City. Address: 217 Hong Bang Street, Ward 11, District 5, Ho Chi Minh City, Viet Nam
- Pham Ngoc Thach University of Medicine. Address: 2 Duong Quang Trung Street, Ward 12, District 10, Ho Chi Minh City, Viet Nam
- School of Biomedical Engineering, International University, Viet Nam. Address: Quarter 6, Linh Trung Ward, Thu Duc City, Ho Chi Minh City, Viet Nam
- Vietnam National University Ho Chi Minh City, Ho Chi Minh City, Viet Nam. Address: Linh Trung Ward, Thu Duc City, Ho Chi Minh City, Viet Nam
- Ho Chi Minh University of Banking. Address: 36 Ton That Dam Street, Nguyen Thai Binh Ward, District 1, Ho Chi Minh City, Viet Nam
Abstract
Introduction: This pilot study aimed to evaluate the feasibility of home blood pressure (BP) telemonitoring among older Vietnamese adults with mild cognitive impairment (MCI) and uncontrolled hypertension in a Geriatrics clinic in Viet Nam. The recruitment (83.8%) and retention (64.5%) rates demonstrate moderate feasibility; however, significant barriers — such as technical reliability and patient non-adherence — were identified. This study underscores the critical challenges of real-world implementation and offers insights for enhancing future telemonitoring interventions for this vulnerable population.
Methods: The control group received standard care, which included adhering to medication prescriptions and attending routine monthly clinic visits for blood pressure monitoring. The locally developed BP telemonitoring device, previously validated at Viet Nam National University, showed an accuracy comparable to international standards. For participants with MCI, caregivers were involved in the consent process to ensure ethical safeguards and full comprehension of study procedures. We conducted a two-arm pilot study. Eligible older patients with MCI and uncontrolled hypertension were invited to participate. Patients were allocated to the intervention group if they were interested in BP telemonitoring; otherwise, they were placed in the control group. Patients were trained to measure their home BP and followed up for three months. Alerts were generated when there were insufficient BP readings.
Results: We invited 74 eligible patients, but 12 declined participation. Overall, 62 participants were allocated to the telemonitoring group (n = 31) or the usual care group (n = 31). The recruitment rate was 83.8%, and the retention rate was 64.5%. The most common reason for withdrawing was “telemonitoring BP devices did not work properly” (45.4%). Alerts were triggered in 22 patients (70.9%), and over 80% of these alerts resulted from patient non-adherence and system problems. After three months, systolic BP was lower in both the intervention group and the control group compared to systolic BP at baseline (telemonitoring group, 137.1 [14.5] mm Hg vs. control group, 143.1 [18.8] mm Hg). No significant difference was observed between the two groups (adjusted mean difference −1.58 mm Hg [95% CI −19.25 to 16.08]).
Conclusions: This pilot study demonstrated the feasibility of home BP telemonitoring in older Vietnamese adults with MCI and uncontrolled hypertension. However, technical reliability and patient adherence issues must be addressed before wider-scale implementation. Future research with a larger sample size and a longer follow-up period is necessary to confirm these findings.
Introduction
Hypertension is a significant risk factor for cognitive impairment and dementia, which is one of the leading causes of death and disability in older adults1, 2. Indeed, hypertension significantly increases the risks of stroke, microbleeds, cerebral white matter lesions, and vascular dementia3. In a cohort study on approximately 430,000 people, it was shown that in individuals aged 60–69 years, per 10 mmHg systolic blood pressure (SBP), the risk of dementia increased by 8%4. According to the World Health Organization, BP control is one of the recommendations for preventing dementia5. A meta-analysis research including six prospective community-based studies with a sample size of 31,090 participants (aged ≥ 55 years) explored that in hypertensive individuals, using antihypertensive medication decreased the risk of dementia and Alzheimer’s disease by 12% and 16%, respectively, compared to those without using antihypertensive medication4, 6. Apparently, treatment of hypertension based on controlling blood pressure plays a critical role in protecting cognition.
Viet Nam, a fast-aging country, is predicted to become an aged country in 20357, with the prevalence of dementia in older adults in the community and hospitals reported at 9.4%8 and 24.3%9, respectively. The prevalence of hypertension among Vietnamese older people was also significantly high (62.1%), resulting in stroke as the leading cause of death and disability10. However, only 12.2% of hypertensive patients had controlled BP11. Therefore, controlling BP in older adults, particularly in those with mild cognitive impairment may prevent them from dementia12. One effective method for BP measurements is using home BP telemonitoring. Compared to office BP measurements, home BP monitoring presents several advantages such as reducing masked uncontrolled hypertension or the white-coat effect13. Moreover, self-measured BP monitoring helps predict cardiovascular outcomes and end-organ damage14. Previous studies also suggested that home BP telemonitoring via the internet or phones promoted antihypertensive medication adjustments faster and enhanced BP control15, 16. However, we lack data on BP telemonitoring in older adults with MCI in Viet Nam.
In this study, we aimed to evaluate the feasibility of home BP telemonitoring in older adults with mild cognitive impairment in an outpatient clinic in Ho Chi Minh City. We evaluated the feasibility of home BP telemonitoring through the rate of recruitment, the rate of participant retention, and patient adherence via the number and types of alerts. The purpose of this study is to examine whether home blood pressure telemonitoring is feasible regarding patient adherence or system problems and to introduce BP telemonitoring as an effective tool for controlling blood pressure.
Methods
Study design
A pilot study was conducted at the Geriatric Outpatient Clinic of Ho Chi Minh City University Medical Center, a university hospital located in District 5 in Ho Chi Minh City, Viet Nam. We collected data between November 2021 and May 2022. The study was approved by the Institutional Review Board of the University of Medicine and Pharmacy at Ho Chi Minh City (approval number: 301/HĐĐĐ-ĐHYD).

Patient flow diagram. The study recruited patients aged ≥ 60 years. Eligible participants expressing interest were enrolled. Reasons for exclusion are noted. Participants were allocated to either the Intervention Group or the Control Group. Both groups underwent a 3-month follow-up period with monthly office blood pressure (BP) monitoring using a blood pressure device.
Participants
The inclusion criteria were: (1) aged ≥ 60 years; (2) confirmed diagnosed with primary hypertension based on ESC/ESH Guideline17, identified from the Geriatric Outpatient Clinic, and having uncontrolled blood pressure (SBP ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg at the clinic visit or at home), or newly diagnosed with primary hypertension; (3) mild cognitive impairment, screened by the Montreal Cognitive Assessment (MoCA) test (a total score < 26)18; (4) equipped with wireless internet at home and interested in participating in the intervention and willing to participate in the study.
The exclusion criteria were: (1) diagnosed with dementia according to DSM-519 or (2) severe vision or hearing impairment or (3) the arm circumference > 32 cm or < 22 cm (cuff size available to allow measurements in arms) or (4) not able to take BP measurements at home or (5) atrial fibrillation was excluded due to its impact on oscillometric BP measurement accuracy, which can compromise data reliability in telemonitoring systems (Figure 1).
Procedures
Older patients in the Outpatient Geriatric Clinic during the study period were screened for eligibility. We then explained the study to eligible participants. If they were interested in participating in the study, written informed consent was provided. Given participants’ MCI, caregivers were involved in the consent process to ensure ethical comprehension and voluntary participation, according to local ethical guidelines and international best practices. All patients participating in the study were thoroughly explained about the research process and fully understood the study before signing the consent form in the presence of a family member. All participant information is encrypted and stored in a password-protected computer, with access limited to the researchers only. Due to the nature of the intervention, neither the patients nor the physicians were blinded to the patient’s group assignment. However, outcome assessors and data analysts were blinded. Each participant in the intervention group received a telemonitoring BP device whereas those in the control group received usual care which included taking medications as prescribed and attending routine monthly clinic visits for blood pressure monitoring. All participants were followed up for 3 months.
We also recorded participants’ demographic characteristics including age, sex, educational attainment, living status, income status, comorbidity, polypharmacy, smoking, and physical exercise. Polypharmacy was defined as having ≥ 5 types of medicine concurrently20. Meanwhile, physical exercise was defined when a participant had at least 150 minutes of moderate-intensity aerobic activity per week21.
BP monitoring device
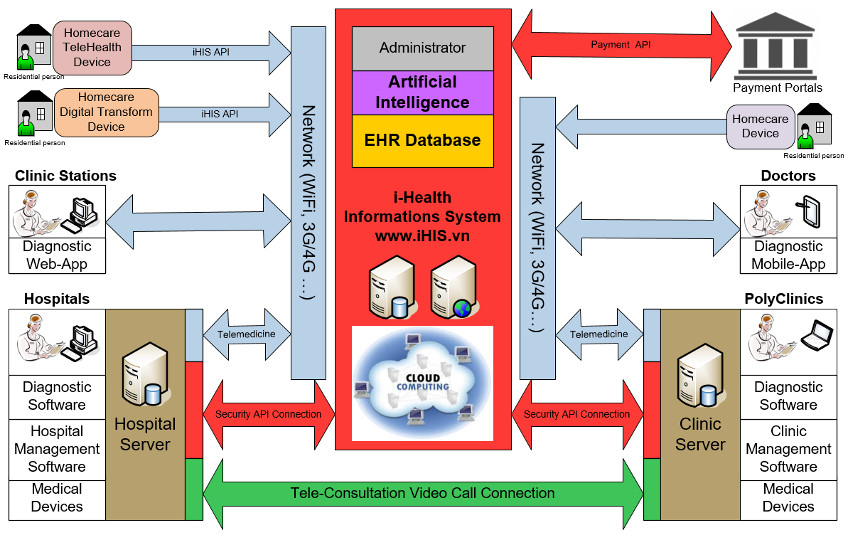
The telemonitoring blood pressure device was developed by the International University - Viet Nam National University Ho Chi Minh City (Model: IUBME_TBP001). It is an automatic BP measuring device with an upper-arm model, including a cuff placed on the upper arm and connected to the monitor by a tube. The monitor is rested on a surface near the arm. Its use is simple with one button START/STOP. This telemonitoring blood pressure device measures and displays systolic blood pressure (SBP), diastolic blood pressure (DBP), and pulse, wirelessly transmitting this data to the cloud-based health information system (iHIS) for analysis and storage. Each user has an account on the iHIS database. The iHIS system connects to home monitoring devices via an HL7-based iHIS API, encrypting data with AES (Advanced Encryption Standard) for secure storage in the user's account on the cloud server. The device connects to the Internet via WiFi (10-20 meter range) and its rechargeable Li-ion battery supports approximately 80 measurements per full charge. The monitor features a 0-240 mmHg (±5 mmHg accuracy) blood pressure range, a 40-180 bpm (±3 bpm accuracy) heart rate range, an LCD touchscreen for user selection and WiFi setup, and performs fully automatic measurements on the upper arm. Users can reset or reconnect the device if uploads fail, with phone/message support available. The safety, quality, and compliance of this device as well as the whole telemonitoring BP system, were approved and certified by the official agency of the Ministry of Information and Communications in Viet Nam (approval number: 0006_18/HAKDT/BBKT).
The cloud telemedicine information system was managed by an administrator (a research member), who was able to monitor, store, and process data and permit users to check the patient’s data using a smartphone or a computer. If the patient has abnormal BP (SBP>180 or DBP>110), a warning sign will alarm a geriatrician (a research member). Both this device and the system were used in a controlled study conducted and proven for their reliability in Viet Nam22.
Home blood pressure monitoring training
For the intervention group, two research members (a geriatrician and a technician) trained participants or their caregivers to use the BP telemonitoring device. The intervention group consisted of patients with uncontrolled blood pressure; therefore, the study followed the frequency and duration of blood pressure measurements as recommended by the International Society of Hypertension, and the American Heart Association and American Medical Association guidelines to adjust treatment for patients14, 23. They were instructed to take three BP readings daily and a minimum of three consecutive days per week to ensure adequate clinical decision-making data14. In case we did not receive BP readings for two consecutive weeks, we would contact participants to identify the reasons. Participants and their caregivers were instructed when they contact research staff or what to do when patients had high BP readings (SBP ≥ 180 mmHg or DBP ≥ 110 mmHg).
Alert manager
The alerts were automatically generated when patients had insufficient BP readings (<4 consecutive days for two weeks). We classified the alerts into five categories: (1) patient non-adherence - the patients or their caregivers did not follow the research protocol; (2) patient knowledge - the patients did not know how to use the telemonitoring BP device; (3) device problem - the devices did not work properly; (4) system problem - the patients took sufficient BP readings but the data were not transmitted to the central server; (5) others such as the patients were hospitalized or on vacations.
Outcome measurements
The feasibility of telemonitoring BP included (1) the rate of participant recruitment, (2) the rate of participant retention, and (3) the number and types of alerts from the BP telemonitoring devices.
The rate of participant recruitment was the percentage of participants agreeing to participate in the study. The rate of participant retention was the percentage of participants remaining until the end of the study.
The primary outcome was clinic-measured blood pressure, adjusted for baseline covariates at 3 months. Blood pressure was measured by an investigator using a validated monitor, three times at baseline and each follow-up appointment in a standardized fashion, using the same arm and cuff size each time, in a seated position after at least 5 min rest.
Data analysis
We analyzed data using STATA/MP software version 14.0 (StataCorp, USA). Continuous variables were presented as mean ± standard deviation (SD) or median and interquartile range. Discrete variables were presented as counts and percentages. T-tests were used to compare the means of two groups; Chi-square tests or Fisher exact tests were used to compare proportions, and a p ≤ 0.05 was considered statistical significance.
Characteristicsof participants in the study (n = 62)
|
Characteristics |
The telemonitoring group (n = 31) |
The control group (n = 31) |
p |
|---|---|---|---|
|
Age (mean±SD) |
72.35 ± 7.76 |
71.67 ± 7.34 |
0.725 |
|
Age group (years) | |||
|
60 – 69 |
14 (45.16) |
14 (45.16) |
0.753 |
|
70 – 79 |
11 (35.48) |
13 (41.94) | |
|
≥ 80 |
6 (19.35) |
4 (12.90) | |
|
Sex | |||
|
Women |
22 (70.97) |
20 (64.52) |
0.587 |
|
Men |
9 (29.03) |
11 (35.48) | |
|
Educational level | |||
|
Primary school |
14 (45.16) |
16 (51.61) |
0.871* |
|
Secondary school |
9 (29.03) |
10 (32.26) | |
|
High school |
6 (19.35) |
4 (12.90) | |
|
University/Post-graduate |
2 (6.45) |
1 (3.23) | |
|
Living status | |||
|
Alone |
1 (3.23) |
5 (16.13) |
0.195* |
|
With family members |
30 (96.77) |
26 (83.87) | |
|
Income status | |||
|
From employment |
0 |
2 (6.45) |
0.671* |
|
From children |
15 (48.39) |
16 (51.61) | |
|
From saving money |
11 (35.48) |
9 (29.03) | |
|
From pension |
5 (16.13) |
4 (12.90) | |
|
Comorbidities | |||
|
Stroke |
5 (16.13) |
6 (19.35) |
0.740 |
|
Ischemic heart disease |
10 (32.26) |
11 (35.48) |
0.788 |
|
Heart failure |
2 (6.45) |
7 (22.58) |
0.147* |
|
Diabetes |
12 (38.71) |
15 (48.39) |
0.442 |
|
Dyslipidemia |
20 (64.52) |
25 (80.65) |
0.155 |
|
Peripheral arterial disease |
0 |
2 (6.45) |
0.151* |
|
Polypharmacy (yes) |
20 (64.52) |
19 (63.33) |
0.923 |
|
Smoking (yes) |
4 (12.90) |
2 (6.45) |
0.671* |
|
Physical exercise (yes) |
19 (61.29) |
26 (83.87) |
0.046 |
Results
Study population
From 310 patients screened, 94 patients (30.3%) had met inclusion criteria, 20 patients were excluded, then 31 patients were enrolled in the intervention group and 31 patients in the control group (Figure 2).
The rate of participant recruitment
During the study period, we invited a total of 74 eligible patients but 12 refused to participate; hence, the rate of recruitment was 83.8%. The reasons for refusing participation included having a home BP monitor (7/12), the BP monitoring protocol being complicated (2/12), not revisiting the Geriatrics Clinic (2/12), and the telemonitoring BP system being quite complicated (1/12) (Figure 2).
Characteristics of the patients in the intervention group stratified by alerts (n = 28)
|
Characteristics |
≤ 2 alerts |
> 2 alerts (n = 23) (%) |
p |
|---|---|---|---|
|
Age (mean ± SD) |
66 ± 3.16 |
73.09 ± 6.84 |
0.003* |
|
Age group (years) | |||
|
60 – 69 |
4 (80) |
9 (39.1) |
0.225* |
|
70 – 79 |
1 (20) |
9 (39.1) | |
|
≥ 80 |
0 |
5 (21.8) | |
|
Sex | |||
|
Women |
4 (80) |
17 (73.9) |
0.776* |
|
Men |
1 (20) |
6 (26.1) | |
|
Educational level | |||
|
Primary school |
3 (60) |
10 (42.5) |
0.863* |
|
Secondary school |
1 (20) |
6 (26.1) | |
|
High school |
1 (20) |
5 (21.7) | |
|
University/Post-graduate |
0 |
2 (8.7) | |
|
Living status | |||
|
Alone |
0 |
1 (5.9) |
0.635* |
|
With family members |
5 (100) |
22 (94.1) | |
|
Income status | |||
|
From employment |
0 |
0 |
0.160* |
|
From children |
4 (80) |
9 (39.1) | |
|
From saving money |
0 |
10 (43.5) | |
|
From pension |
1 (20) |
4 (17.4) | |
|
Comorbidities | |||
|
Stroke |
2 (40) |
3 (13) |
0.120* |
|
Ischemic heart disease |
3 (60) |
7 (30.4) |
0.315* |
|
Heart failure |
1 (20) |
1 (4.3) |
0.331* |
|
Diabetes |
2 (40) |
9 (39) |
1* |
|
Dyslipidemia |
5 (100) |
18 (78.3) |
0.550* |
|
Peripheral arterial disease |
0 |
0 |
0 |
|
Polypharmacy (yes) |
5 (100) |
13 (56.2) |
0.066* |
|
Smoking (yes) |
2 (40) |
2 (8.7) |
0.070* |
|
Physical exercise (yes) |
4 (80) |
15 (65.2) |
0.253* |

Flow of participants through the study. Diagram showing the screening, enrollment, and allocation process for hypertension patients aged ≥ 60 years with uncontrolled hypertension and mild cognitive impairment (MCI).
The rate of participant retention
In the intervention group (n = 31), 11 patients withdrew from the study. Therefore, the rate of participant retention was 64.5% (
Number and types of alerts
During the 3-month follow-up, 28 patients used BP devices and transmitted at least one BP reading to the central server. 70 alerts were recorded from 22 patients (70.9%). At the end of the study, 5 (17.9%) patients had ≤ 2 alerts whereas 23 (82.1%) patients had > 2 alerts. Types of alerts are presented in
Number and types of alerts
|
Types of alerts |
n |
% |
|---|---|---|
|
Patient non-adherence |
32 |
45.7 |
|
Patient knowledge |
3 |
4.3 |
|
Device problem |
5 |
7.1 |
|
System problem |
25 |
35.7 |
|
Others (on vacation, hospitalization) |
5 |
7.1 |
Mean blood pressure at baseline, 1 month, and 3 months for each group
|
|
Baseline (T0) |
1 month (T1) |
3 months (T2) |
1-month adjusted means difference (95% CI, p-value) |
3-month adjusted means difference (95% CI, p-value) |
|
Systolic blood pressure mmHg | |||||
|
Telemonitoring group |
163.3 ± 9.4 |
146.5 ± 20.1 |
137.1 ± 14.5 |
-2.22 (-12.81 to 8.36), p = 0.6746* |
-1.58 (-19.25 to 16.08), p = 0.856* |
|
Control group |
160.2 ± 16.1 |
147.2 ± 21.5 |
143.1 ± 18.8 | ||
|
Diastolic blood pressure mmHg | |||||
|
Telemonitoring group |
88 ± 12.8 |
79.7 ± 13.5 |
74.5 ± 8.2 |
-1.37 (-8.28 to 5.55), p = 0.6938* |
-4.04 (-14.17 to 6.08), p = 0.422* |
|
Control group |
90.4 ± 12 |
82 ± 11.1 |
80.8 ± 10.9 | ||
Blood pressure measurement
Mean blood pressure at baseline, 1 month, and 3 months in two groups
|
|
Baseline (T0) |
1 month (T1) |
3 months (T2) |
1-month adjusted means difference (95% CI, p-value) |
3-month adjusted means difference (95% CI, p-value) |
|
Systolic blood pressure mmHg | |||||
|
Telemonitoring group |
163.3 ± 19.4 |
146.5 ± 20.1 |
137.1 ± 14.5 |
-16.9 (-23.36 to -10.45), p < 0.001* |
-23.46 (-31.24 to -15.69), p < 0.001* |
|
Control group |
160.2 ± 16.1 |
147.2 ± 21.5 |
143.1 ± 18.8 |
-12.67 (-20.18 to -5.18), p = 0.0018* |
-23.5 (-37.22 to -9.77), p = 0.0017* |
|
Diastolic blood pressure mmHg | |||||
|
Telemonitoring group |
88 ± 12.8 |
79.7 ± 13.5 |
74.5 ± 8.2 |
-8.35 (-13.08 to -3.63), p = 0.001* |
-11.23 (-15.88 to -6.58), p < 0.001* |
|
Control group |
90.4 ± 12 |
82 ± 11.1 |
80.8 ± 10.9 |
-8.32 (-13.29 to -3.35), p = 0.0019* |
-14.84 (-22.65 to -7.03), p < 0.001* |
Discussion
This study evaluated the feasibility of BP telemonitoring in older Vietnamese patients with mild cognitive impairment and uncontrolled hypertension. The results showed that the rate of recruitment and participant retention was 83.8% and 64.5%, respectively. Approximately 80% of participants had alerts, and the majority of alerts were due to system problems and patient non-adherence.The rate of recruitment in our study was significantly high, which showed that older people tend to care about their BP monitoring. This can be explained in Viet Nam, recently, health promotion programs and available online health information have been helping to raise public awareness, including hypertension and its related complications, which might contribute to improving health knowledge and decision-making in older adults in Viet Nam24, 25. Besides, in this study, most of the eligible participants refused to participate because they already owned home BP monitoring devices.The rate of retention in our study was relatively significant (64.5%). Approximately 73% (72.7%) of withdrawing participants were due to technical device and technical system problems. Therefore, improving these issues may help boost the rate of patients in a larger study in the future. In a previous study on patients with poor BP control, technical problems were also a critical concern in BP telemonitoring26. The relatively high recruitment rate highlights a growing awareness of hypertension and self-care among older Vietnamese adults. However, the dropout rate in the intervention group (35.5%) underscores the need for system improvements. Technical issues, including device malfunction and Wi-Fi disconnection, were the most frequently cited causes of withdrawal. The problem stemmed from the blood pressure devices failing to connect to Wi-Fi and the server losing signal because of power outages at the International University’s server location. Therefore, upgrading the system and improving these issues may improve patient adherence to home BP monitoring. On the other hand, future telemonitoring systems should consider cellular-based data transmission or local storage with delayed upload to improve reliability in similar settings. This will help hypertensive patients improve BP control and reduce the risks of hypertension-related complications as well as the risk of dementia among older adults.However, approximately 27.3% of withdrawing patients in our study reported BP measuring protocol was complicated and they could not follow it. Besides, alerts related to non-adherence accounted for 45.7% of all alerts, indicating difficulty in maintaining the required frequency of BP measurements. Hence, implementing self-measured BP monitoring according to the American Heart Association and American Medical Association guidelines (measuring BP ≥ 3 days/week) on hypertensive patients remains a barrier in reality14. Patient adherence posed another significant barrier. This challenge may be attributed to protocol complexity and the cognitive limitations of the population studied. Adjusting the protocol to allow fewer weekly (once to twice per week) measurements or caregiver-assisted monitoring could enhance compliance. In clinical practice, most of the patients visiting the Geriatrics Clinic reported that they seldom measure their home BP. It implies the importance of general practitioners in recommending self-measured BP monitoring among hypertensive patients.Given the cognitive limitations associated with MCI, caregiver involvement plays a critical role in enhancing adherence to telemonitoring protocols. They can provide hands-on assistance with the use of BP devices, help maintain routine measurement schedules, and facilitate communication between patients and healthcare providers. In our study, while caregiver support was part of the initial training and consent process, more structured and ongoing involvement may be necessary to sustain adherence. Therefore, future telemonitoring interventions should explicitly integrate caregiver engagement into study protocols, including training modules tailored for caregivers, clear task-sharing guidelines, and digital support tools such as caregiver reminder systems or app-based monitoring dashboards. Empowering caregivers with the skills and tools to assist in telemonitoring could not only improve protocol compliance but also enhance patient safety by ensuring that abnormal BP readings are promptly addressed. Additionally, recognizing and addressing caregiver burden through appropriate support mechanisms will be essential for the sustainability of such interventions in real-world settings.This study has shown that the proportion of patients with out-of-range BP values was higher in the control group than in the telemonitoring group. Using self-monitoring of blood pressure in primary care resulted in lower mean blood pressure compared with usual care. Because of telemedicine solutions, doctors can follow the patients outside their office, track their health status, and easily and quickly communicate with them, a particularly important feature in cases of acute symptoms or sudden BP rises. The effect of HBPT in conjunction with cointervention (including for instance medication titration by a case manager, education, or lifestyle counseling) led to significantly larger BP reductions than self–BP monitoring alone without transmission of BP data and counseling, suggesting a possible additional effect of the HBPT approach beyond self–BP monitoring.While initial setup costs for telemonitoring systems may be high, long-term benefits such as reduced clinic visits, improved BP control, and fewer complications may offset these expenses. Future research should formally assess cost-effectiveness, particularly in resource-limited settings.Our study also has several limitations. Importantly, this study was not randomized, which may restrict generalizability and introduce selection bias. Additionally, the small sample size limited statistical power and prevented the detection of subtle effects on BP outcomes. These limitations must be addressed in future research by implementing randomized controlled trials with larger populations and extended follow-up. Besides, a high dropout rate in the intervention group, primarily due to device and system failures, raises concerns about the intervention’s practicality. Finally, the frequency of BP measurements in the protocol may not be suitable for older adults with MCI. However, this was the first study to evaluate the feasibility of telemonitoring blood pressure in older patients with mild cognitive impairment. It will serve as a cornerstone for developing a larger randomized controlled trial with an extended follow-up duration to assess the effectiveness of telemonitoring blood pressure in older patients, which can help improve blood pressure control and reduce hypertension-related complications in older Vietnamese adults.This study revealed significant real-world barriers to telemonitoring implementation, particularly related to technical reliability and protocol complexity. To improve adherence, future improvements should focus on enhancing wireless connectivity, simplifying device interfaces, reducing the frequency of BP measurements, and enhancing caregiver support. More actively involving caregivers may also help mitigate non-adherence issues. Additionally, the wide confidence intervals observed in BP differences highlight the need for a larger sample size to improve statistical precision.
Conclusions
Home BP telemonitoring is feasible among older Vietnamese patients with MCI and uncontrolled hypertension, though implementation is challenged by technical and adherence issues. To improve feasibility and scalability, future interventions should include more robust and user-friendly technologies, alternative measurement protocols, and increased caregiver involvement. Scaling up these interventions in Viet Nam will require both technological improvements and strong primary care engagement to promote patient and caregiver participation in self-monitoring. To address adherence issues, general practitioners, as well as cardiologists and geriatricians, should explain the benefits of self-measured BP monitoring for hypertensive patients to enhance BP control in these individuals.
Abbreviations
AES: Advanced Encryption Standard, API: Application Programming Interface, BP: Blood Pressure, CI: Confidence Interval, DBP: Diastolic Blood Pressure, DSM-5: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, ESC: European Society of Cardiology, ESH: European Society of Hypertension, HL7: Health Level Seven, iHIS: Cloud-based Health Information System, Li-ion: Lithium-ion, MCI: Mild Cognitive Impairment, MoCA: Montreal Cognitive Assessment, SBP: Systolic Blood Pressure, SD: Standard Deviation, WHO: World Health Organization, and Wi-Fi: Wireless Fidelity
Acknowledgments
We would like to thank all the participants and our colleagues for their support during the project.
Author’s contributions
Vy Le Tran: Collaborated in the design of the article, methodology, data analysis, and writing of the article. Tran To Tran Nguyen: Collaborated in the design of the article, data analysis, writing, and review of the article. Dinh Bao Chau Hoang: Collaborated in writing and review of the article. The Ngoc Ha Than: Collaborated in the design of the article, writing, and review of the article. Tuan Chau Nguyen: Collaborated in monitoring the analysis, writing, and review of the article. Viet Ngoc Tran: Collaborated in the methodology, supervision, and review of the article. Toi Van Vo: Collaborated in the design of the article, monitoring of analysis, and review of the article. Nam Phuong Nguyen: Collaborated in the design of the article, supervision of the information system, and review of the article. Huong Thanh Thi Ha: Collaborated in the design of the article, monitoring of analysis, supervision, writing, review, and editing of the article. All authors read and approved the final manuscript.
Funding
This work was funded by the Global Challenges Research Fund Networking Grant (GCRF) project number GCRFNGR6
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the University of Medicine and Pharmacy at Ho Chi Minh City. All participants provided informed consent prior to their inclusion in the study.
Consent for publication
Not applicable.
Declaration of generative AI and AI-assisted technologies in the writing process
During the preparation of this work, the authors used Grammarly to eliminate spelling, grammar, and punctuation mistakes. After using this tool, the authors reviewed and edited the content as needed and took full responsibility for the content of the publication.
Competing interests
The authors declare that they have no competing interests.

